Syphilis Stages Explorer
Primary Syphilis
3 weeks after exposure
Secondary Syphilis
2-8 weeks after primary
Latent Syphilis
Weeks to years
Tertiary Syphilis
Years (often >3)
Syphilis Timeline Progression
Stage Details
Select a stage above to learn more about its characteristics, symptoms, and treatment.
Important Notes
- Early stages (primary and secondary) are highly treatable with a single dose of penicillin
- Latent syphilis shows no symptoms but still requires treatment to prevent damage
- Tertiary syphilis can cause irreversible damage to vital organs
- Congenital syphilis can be prevented with early prenatal screening
Quick Summary / Key Takeaways
- Syphilis moves through syphilis stages that each have distinct signs and timeframes.
- Early stages (primary and secondary) are usually easy to treat with a single dose of penicillin.
- Latent syphilis shows no symptoms but still requires treatment to prevent damage later on.
- Tertiary syphilis can affect the heart, brain, and bones and may need longer antibiotic courses.
- Pregnant people can pass the infection to their baby, causing congenital syphilis, which is preventable with early screening.
What Is Syphilis?
Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. The disease has a reputation for being called “the great imitator” because its symptoms can mimic many other conditions. If left untreated, the infection follows a predictable path of worsening health problems, which is why understanding each stage matters.
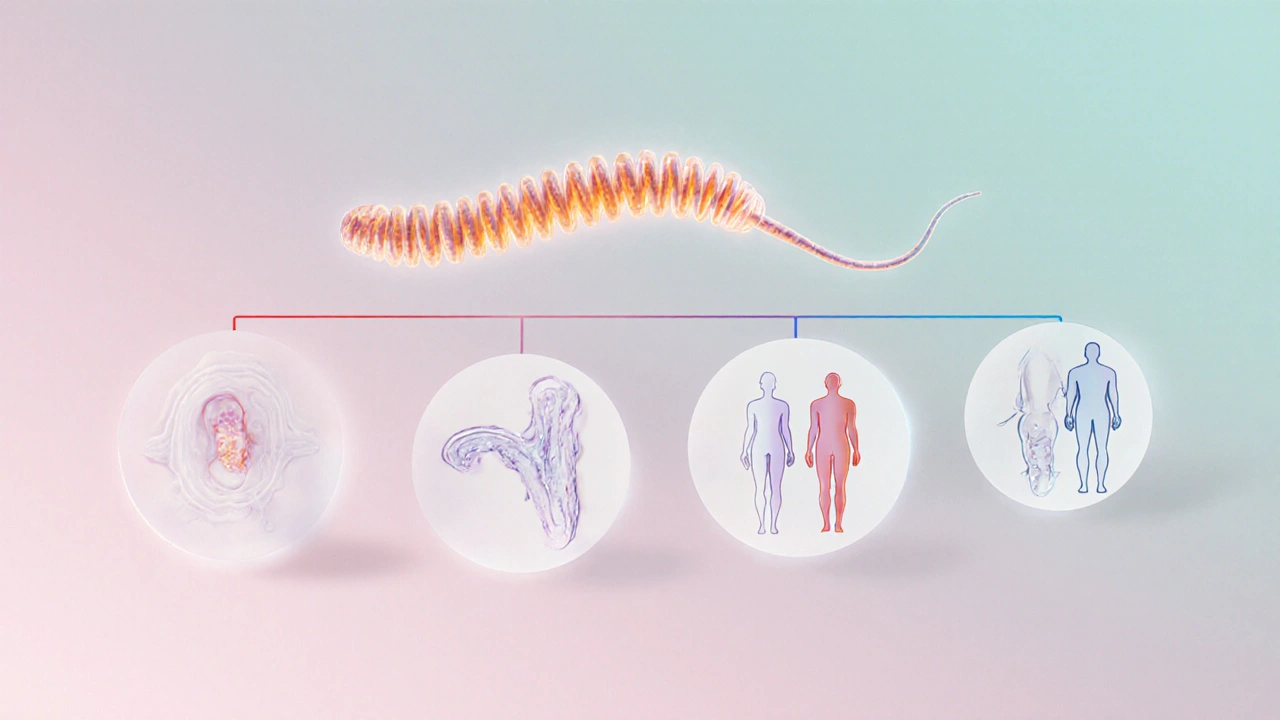
How Syphilis Progresses: The Stages
After infection, the bacteria travel through the bloodstream and settle in different tissues. Over weeks to years, the disease unfolds in several phases, each with its own clinical picture. Knowing the timeline helps you recognize warning signs early and seek treatment before irreversible damage occurs.
Primary Syphilis
Primary syphilis appears about three weeks after exposure. The hallmark is a single, painless sore called a chancre, usually on the genital area, anus, or mouth. The sore heals on its own in 3‑6 weeks, but the bacteria remain alive underneath.
- Typical location: genitals, rectum, lips.
- Size: 0.5-2cm, firm and round.
- Accompanying signs: mild swollen lymph nodes nearby.
Because the chancre feels harmless, many people ignore it, allowing the infection to slip into the next stage.

Secondary Syphilis
Secondary syphilis kicks in 2-8 weeks after the chancre resolves. This phase is marked by a widespread rash that can involve the palms and soles-something few other STIs do. Other symptoms include fever, sore throat, hair loss, and muscle aches.
- Rash pattern: copper‑colored spots, often non‑itchy.
- Systemic signs: low‑grade fever, malaise.
- Mucous‑membrane lesions: moist patches on the mouth or genitals.
These manifestations usually disappear within a few weeks, yet the infection silently moves forward.
Latent Syphilis
Latent syphilis is the silent middle ground. After secondary symptoms fade, the disease enters a period with no visible signs. Doctors split it into early latent (within the first year) and late latent (beyond a year). Blood tests stay positive, but patients feel fine.
- Early latent: still contagious; risk of progressing to tertiary disease.
- Late latent: no longer infectious, but organ damage can still develop.
Without treatment, about one‑third of people will eventually move to the final stage.
Tertiary Syphilis
Tertiary syphilis can surface years-sometimes decades-after the initial infection. It attacks internal organs and may cause:
- Cardiovascular problems (aortitis, aneurysm).
- Neurological damage (general paresis, tabes dorsalis).
- Destructive skin or bone lesions called gummas.
At this point, the damage is often irreversible, emphasizing why early detection matters.
Congenital Syphilis
Congenital syphilis occurs when a pregnant person transmits the bacteria to the fetus. Babies can be born with rash, fever, organ enlargement, or even stillbirth. The good news: routine prenatal screening and prompt penicillin treatment can prevent almost all cases.
Diagnosis and Testing
Doctors rely on blood tests to confirm infection. The most common are:
- Rapid plasma reagin (RPR) - a non‑treponemal test that measures antibodies produced in response to the infection.
- Venereal Disease Research Laboratory (VDRL) - another screening test with similar purpose.
- Confirmatory treponemal tests (FTA‑ABS, TP‑PA) that detect antibodies specific to Treponema pallidum.
Positive screening followed by a confirmatory test gives a definitive diagnosis. Testing is recommended for anyone with risk factors or unexplained symptoms.

Treatment Overview
Penicillin remains the gold‑standard therapy for all syphilis stages. The regimen varies:
- Primary, secondary, or early latent: a single intramuscular dose of benzathine penicillin G (2.4million units).
- Late latent or tertiary without neurosyphilis: three weekly doses of the same amount.
- Neurosyphilis or pregnant patients: intravenous aqueous crystalline penicillin for 10‑14 days.
For those allergic to penicillin, doxycycline or ceftriaxone may be alternatives, but they are less studied in pregnancy.
Prevention Tips
- Use condoms consistently; while they don’t eliminate risk completely, they drastically reduce it.
- Get tested regularly if you have multiple partners or engage in high‑risk activities.
- Pregnant individuals should undergo syphilis screening at the first prenatal visit and again in the third trimester if at risk.
- Inform sexual partners if you test positive so they can seek testing and treatment.
- Avoid sharing needles or other equipment that could introduce blood into the body.
Comparison of Syphilis Stages
| Stage | Typical Time After Infection | Main Symptoms | Contagious? | Standard Treatment |
|---|---|---|---|---|
| Primary | ~3 weeks | Single painless chancre | Yes | Single 2.4MU penicillin dose |
| Secondary | 2-8 weeks after primary | Rash (palms/soles), fever, mucous‑membrane lesions | Yes | Single 2.4MU penicillin dose |
| Latent | Weeks to years | No visible signs | Early latent: Yes; Late latent: No | Three weekly 2.4MU doses (late) |
| Tertiary | Years (often >3) | Cardiovascular, neurological, or gummatous lesions | No | Three weekly 2.4MU doses or IV penicillin for neurosyphilis |
Common Misconceptions
1. “If the sore goes away, the infection is cured.” - The chancre heals on its own, but the bacteria remain and can spread.
2. “You can’t get syphilis from oral sex.” - The bacteria can infect the mouth or throat; oral lesions are possible.
3. “Antibiotics other than penicillin work just as well.” - Penicillin is the only drug proven to reliably clear the infection in all stages, especially in pregnancy.
Frequently Asked Questions
Can syphilis be cured without treatment?
No. The bacteria never go away on their own. Even if symptoms disappear, the infection persists and can cause serious damage later.
How long does it take for a test to become positive after exposure?
Screening tests like RPR or VDRL are usually positive 1-3 weeks after infection, but a confirmatory treponemal test can detect antibodies a bit later.
Is syphilis a lifetime infection if left untreated?
Yes. Without antibiotics, the disease progresses through its stages and can lead to irreversible organ damage, but it remains present for life.
Can I still have sex after a single dose of penicillin?
It’s safest to abstain for at least 7 days after treatment and until a follow‑up test shows a drop in antibody levels. This reduces the chance of passing the infection.
What should pregnant people do to avoid congenital syphilis?
Get screened early in pregnancy, repeat testing in the third trimester if at risk, and receive the recommended penicillin regimen immediately if positive.

Naresh Sehgal
October 8, 2025 AT 13:30Listen up-if you brush off that painless sore thinking it’ll vanish on its own, you’re just inviting the later stages to crash the party. Get tested, get treated, and stop the bacteria from marching toward the heart and brain.
Poppy Johnston
October 8, 2025 AT 16:50Hey folks, just wanted to add that the rash on palms and soles is a classic red flag-don’t dismiss it as a simple skin irritation. Early penicillin can knock it out in one shot, so timely screening is a lifesaver.
Johnny VonGriz
October 8, 2025 AT 20:26In addition to what’s been said, it’s worth noting that the serology tests (RPR and VDRL) become reliably positive only after a few weeks, so a repeat test might be necessary if initial results are negative but exposure is suspected. Also, follow‑up titers help ensure the infection is truly cleared.
Real Strategy PR
October 9, 2025 AT 00:20Skipping penicillin is just reckless.
Doug Clayton
October 9, 2025 AT 04:30Seriously, if you think you can wait until symptoms flare up then it’s a bad idea get tested right away and treat fast because the disease doesn’t wait for you
Michelle Zhao
October 9, 2025 AT 09:30When faced with the multifaceted presentation of syphilis, one must adopt a systematic approach that begins with thorough patient history and risk assessment. The primary chancre, though innocuous in appearance, serves as the initial portal of entry for Treponema pallidum and should trigger immediate serologic testing. Subsequent dissemination during the secondary phase manifests as a papular or maculopapular rash, frequently involving the palmar and plantar surfaces, which distinguishes it from many other sexually transmitted infections. Laboratory confirmation at this stage relies on both non‑treponemal and treponemal assays to establish a definitive diagnosis. Early latent infection, while asymptomatic, maintains a degree of infectivity; thus, contact tracing remains a critical public health measure. The transition to late latent status, however, signifies the cessation of transmissibility but does not preclude organ‑specific complications. Tertiary syphilis, emerging years after the initial insult, may present as cardiovascular aneurysms, neurosyphilitic dementia, or gummatous lesions, each requiring specialized diagnostic imaging and cerebrospinal fluid analysis. Penicillin G, administered in dosage regimens calibrated to disease stage, remains the gold standard therapy, with single‑dose benzathine for early disease and multiple weekly injections for late manifestations. For patients with documented penicillin allergy, desensitization protocols are often preferred over alternative antibiotics due to superior efficacy. Monitoring serologic titers at six‑month intervals post‑treatment provides reassurance of microbiologic cure and alerts clinicians to potential reinfection. Pregnant individuals deserve particular vigilance; timely prenatal screening and timely intramuscular penicillin can avert congenital transmission, which otherwise carries high morbidity and mortality. Public education campaigns that emphasize condom use, routine testing, and the non‑visible nature of latent disease are essential components of prevention. Moreover, clinicians should counsel patients on the necessity of abstaining from sexual activity for at least seven days after therapy until follow‑up testing confirms seroreduction. The psychological impact of a syphilis diagnosis should not be overlooked, as stigma can hinder disclosure and adherence to treatment. Collaborative care involving infectious disease specialists, primary care providers, and mental health professionals optimizes outcomes. Ultimately, a proactive stance that integrates early detection, appropriate antimicrobial therapy, and comprehensive follow‑up offers the best prospect for preventing the irreversible sequelae of this historically notorious “great imitator”.
Eric Parsons
October 9, 2025 AT 15:03Adding to the comprehensive overview, note that neurosyphilis can present subtly with personality changes or gait disturbances, so a lumbar puncture is warranted when neurological signs appear. Also, serologic non‑reactive results after treatment don’t always mean cure; the trend in titers matters more than a single value.
Mary Magdalen
October 9, 2025 AT 21:26The whole “just a rash” excuse is absurd; it’s a red flag that screams infection. If you ignore it, you’re practically inviting a heart‑attack in your twenties.
Dhakad rahul
October 10, 2025 AT 04:56Whoa, drama alert! 🤦♂️ Ignoring a rash is like skipping your own birthday cake – you’re missing the whole point! 😅
William Dizon
October 10, 2025 AT 11:53Great discussion, everyone. Remember, regular testing and prompt treatment keep us all healthier and the spread in check.