Why phenytoin is different from other seizure meds
Phenytoin has been used since the 1930s to control seizures, and it’s still one of the most common drugs for epilepsy. But unlike most other medicines, you can’t just swap it out for a cheaper generic version and expect the same result. The reason? Phenytoin has a narrow therapeutic index - meaning the difference between a dose that works and one that’s dangerous is very small. The safe range is 10 to 20 mcg/mL in your blood. Go just a little over, and you risk toxicity: dizziness, uncontrolled eye movements, confusion, even coma. Go under, and seizures come back.
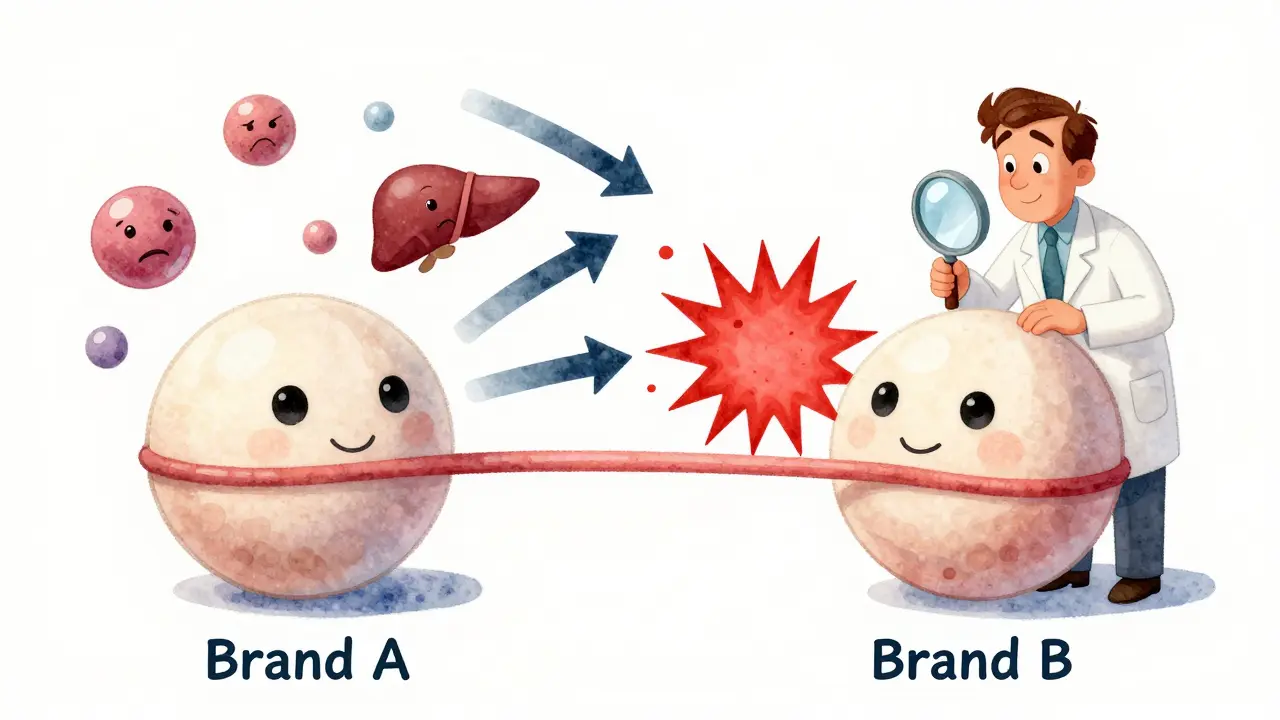
This isn’t just theoretical. In real life, patients have had seizures after switching to a new generic brand. Others ended up in the hospital with tremors and slurred speech because their phenytoin level jumped after a formulation change. The problem isn’t that generics are unsafe - they’re approved by the FDA. It’s that the rules for approval allow up to a 20% variation in how much drug gets into your bloodstream compared to the original brand. For most drugs, that’s fine. For phenytoin, it’s risky.
How phenytoin behaves in your body
Phenytoin doesn’t follow normal rules. Most drugs clear from your body at a steady rate - double the dose, double the level. Not phenytoin. Once your blood level hits around 10 mcg/mL, the enzymes that break it down get overwhelmed. That’s called zero-order kinetics. At that point, a tiny increase in dose - say, 25 mg more - can cause a huge spike in concentration. One patient I saw went from 18 mcg/mL to 42 mcg/mL after adding just one extra 50 mg capsule. He didn’t know why he felt so off until his blood test came back.
Another twist: phenytoin sticks tightly to proteins in your blood - about 90 to 95% of it. Only the 5 to 10% that’s floating free actually works to stop seizures. If you’re malnourished, have liver disease, or are on dialysis, your protein levels drop. Suddenly, even a "normal" total phenytoin level might mean too much free drug is circulating. That’s why checking just the total level can be misleading. In these cases, you need a free phenytoin level - a more accurate but less commonly ordered test.
When switching generics, monitor like clockwork
If you’re on brand-name Dilantin and your pharmacy switches you to a generic, don’t assume everything’s fine. Same if you’re on one generic and get another - even if both are labeled "phenytoin sodium." Different manufacturers use different fillers, coatings, or manufacturing methods. These small differences can change how fast or how much the drug gets absorbed.
Here’s what actually works in practice:
- Get a blood level right before you switch formulations. This is your baseline.
- Don’t take your next dose until after the blood draw. That way, you’re measuring the true trough.
- Wait 5 to 10 days after the switch, then check again. It takes that long for phenytoin to reach a new steady state.
- If the level is outside 10-20 mcg/mL, or if you feel worse - drowsy, shaky, nauseous - call your doctor immediately.
The NHS Tayside guidelines say this isn’t optional. They state clearly: "Therapeutic monitoring may be required when switching formulations." And they’re not alone. The American Academy of Family Physicians says routine monitoring isn’t needed for everyone - but when you switch phenytoin brands, it’s a red flag situation.
What else to watch for - beyond blood levels
Phenytoin doesn’t just affect your brain. Long-term use can mess with your bones, gums, and even your vitamin levels. That’s true no matter which brand you take.
- Gingival hyperplasia: Your gums can swell, bleed, and grow over your teeth. Brushing more won’t fix it. You may need a dentist who knows about this side effect.
- Vitamin D and calcium: Phenytoin speeds up how fast your body breaks down vitamin D. Over time, that leads to low calcium, weak bones, and fractures. Get your vitamin D and ALP levels checked every 2-5 years.
- Blood counts: It can lower your white blood cells or platelets. A simple CBC every 6-12 months catches this early.
- Drug interactions: Common meds like fluconazole, metronidazole, or even antibiotics like sulfa drugs can push phenytoin levels up. Alcohol, seizure drugs like carbamazepine, or rifampin can drop them. Always tell your pharmacist and doctor what else you’re taking.
And if you’re of Han Chinese or Thai descent? Get tested for the HLA-B*1502 gene before starting phenytoin. Carrying this gene increases your risk of a deadly skin reaction called SJS/TEN. It’s rare, but it’s preventable.

What to do if your level is off
If your phenytoin level is too low - say, 7 mcg/mL - and you’re having breakthrough seizures, your doctor might increase your dose. But don’t just add 50 mg. Start with 10-25 mg extra. Wait 5-7 days. Test again. Phenytoin doesn’t respond like insulin or blood pressure meds. It’s slow, unpredictable, and unforgiving.
If your level is too high - above 20 mcg/mL - you might have nystagmus (involuntary eye jerking), trouble walking, or confusion. At 30 mcg/mL, you’re likely unsteady and drowsy. Above 40 mcg/mL, you could be confused or unresponsive. Above 50 mcg/mL, it can be fatal. If you feel this way, don’t wait for your next appointment. Go to the ER. Stop taking phenytoin until you’re evaluated.
And if you’re low on albumin (a protein), your "normal" total level might be hiding a dangerous free level. Ask your doctor: "Should I get a free phenytoin test?" Many labs can do it. It costs more, but it’s worth it if you’re sick, elderly, or have liver disease.
Bottom line: Don’t treat phenytoin like any other pill
Generic phenytoin is cheaper. That’s good. But it’s not interchangeable like ibuprofen or metformin. Every switch - brand to generic, generic to generic - carries risk. The science is clear: for phenytoin, therapeutic drug monitoring isn’t just helpful. It’s essential.
Ask your neurologist or pharmacist: "Am I on a stable formulation?" If you’ve switched brands in the last 30 days, get your level checked. If you’ve been on the same one for years and feel fine? You’re probably okay - but still get your vitamin D and blood counts done yearly. Phenytoin is old, but it’s not simple. Treat it like the powerful, unpredictable drug it is. Your brain and your body will thank you.
Can I switch from brand-name Dilantin to a generic phenytoin without checking my blood levels?
No. Even though generics are FDA-approved, phenytoin’s narrow therapeutic index and nonlinear metabolism mean small changes in absorption can cause toxicity or loss of seizure control. Always check your serum level before and 5-10 days after switching formulations. Clinical guidelines from NHS Tayside and the American Academy of Family Physicians recommend monitoring in these cases.
Why is my phenytoin level normal but I still feel sick?
You may have low albumin (protein) levels due to poor nutrition, liver disease, or kidney issues. Phenytoin is 90-95% bound to proteins. If those proteins drop, more of the drug floats freely - and that’s the active part. A "normal" total level might hide a toxic free level. Ask for a free phenytoin test if you’re symptomatic despite normal total levels.
How often should I get my phenytoin level checked?
After starting or changing dose or formulation, check at 5-10 days for steady state. After that, every 3-6 months if stable. But if you’re elderly, have liver or kidney disease, are on other interacting drugs, or have changed your diet or medications - check sooner. Always test before any formulation switch.
Do I need to worry about bone health if I’m on phenytoin?
Yes. Phenytoin accelerates vitamin D breakdown, leading to low calcium, weak bones, and higher fracture risk over time. Get your vitamin D, calcium, and alkaline phosphatase (ALP) tested every 2-5 years. Many patients don’t know this until they break a bone. Supplements and sun exposure help, but testing is key.
Can I take other medications while on phenytoin?
Some can be dangerous. Antibiotics like metronidazole, antifungals like fluconazole, and even some heart meds like amiodarone can raise phenytoin levels and cause toxicity. Alcohol, seizure drugs like carbamazepine, and rifampin can lower levels and trigger seizures. Always tell every doctor and pharmacist you’re on phenytoin - even for a cold or toothache.
Is there a safer alternative to phenytoin?
Yes - newer antiepileptics like levetiracetam, lamotrigine, or lacosamide have simpler dosing, fewer interactions, and no narrow therapeutic index. But phenytoin is still used because it’s effective and cheap. If you’re stable on it, don’t switch unless there’s a reason. If you’re having side effects or frequent level issues, talk to your neurologist about alternatives.


LALITA KUDIYA
January 7, 2026 AT 19:11Andrew N
January 9, 2026 AT 17:40Poppy Newman
January 10, 2026 AT 18:29Anthony Capunong
January 11, 2026 AT 17:06Vince Nairn
January 13, 2026 AT 07:10Ayodeji Williams
January 14, 2026 AT 13:10Kamlesh Chauhan
January 14, 2026 AT 23:23Alex Danner
January 16, 2026 AT 03:22Jessie Ann Lambrecht
January 16, 2026 AT 03:57Adam Gainski
January 17, 2026 AT 03:58