When you take a medication like warfarin, levothyroxine, or digoxin, even a tiny change in how much of the drug enters your bloodstream can mean the difference between effective treatment and a life-threatening reaction. These are narrow therapeutic index (NTI) drugs - medicines where the gap between a safe dose and a dangerous one is razor-thin. That’s why regulators don’t treat them like regular generics. The bioequivalence standards for NTI drugs are stricter, more complex, and designed with one goal: keeping patients safe.
What Makes a Drug a Narrow Therapeutic Index Drug?
A drug is classified as having a narrow therapeutic index when the difference between the dose that works and the dose that causes harm is very small. The FDA uses a therapeutic index of 3 or less as the cutoff. That means if the toxic dose is only three times higher than the effective dose, it’s considered high-risk. For comparison, most medications have a therapeutic index of 10, 20, or even higher. Common NTI drugs include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Digoxin (heart medication)
- Phenytoin (anti-seizure)
- Tacrolimus and sirolimus (immunosuppressants)
- Lithium carbonate (mood stabilizer)
- Theophylline (asthma medication)
Standard Bioequivalence vs. NTI Bioequivalence
For most generic drugs, regulators accept bioequivalence if the generic’s blood concentration is within 80% to 125% of the brand-name drug. That’s a wide range. For example, if the brand drug reaches 100 ng/mL in the blood, a generic between 80 and 125 ng/mL is considered equivalent. But for NTI drugs, that range is too loose. Imagine two heart transplant patients. One takes a brand-name tacrolimus that keeps their blood level at 12 ng/mL - the sweet spot for preventing rejection without toxicity. The other takes a generic that, because of minor formulation differences, hits 13.5 ng/mL. That 12.5% increase might trigger kidney damage. That’s why regulators tightened the rules. Here’s how the major agencies now handle it:| Regulatory Agency | Acceptance Range for AUC/Cmax | Additional Requirements |
|---|---|---|
| FDA (United States) | 80.00-125.00% (unscaled) + 95-105% (quality assay) | Reference-scaled bioequivalence (RSABE); variability comparison (test/reference ≤ 2.5); fully replicated crossover design |
| EMA (Europe) | 90.00-111.00% | Fixed tightened range; no scaling based on variability |
| Health Canada | 90.0-112.0% | Fixed range for AUC; applies to critical dose drugs |
Why the FDA’s Method Is Different - and More Demanding
The FDA’s reference-scaled average bioequivalence (RSABE) method isn’t just about numbers. It’s about real patient risk. A 2017 study in the American Journal of Transplantation showed that when generic tacrolimus passed the FDA’s NTI criteria, transplant patients had no increase in rejection or toxicity. That’s the proof behind the rules. But it comes at a cost. NTI bioequivalence studies require more participants - usually 36 to 54 people - compared to 24 to 36 for standard generics. They also need more complex study designs, like fully replicated crossover trials, where each patient takes both the brand and generic multiple times. This isn’t just harder to run - it’s more expensive. Industry estimates put the cost of an NTI bioequivalence study at $500,000 to $1 million, compared to $300,000-$700,000 for regular generics. That’s one reason why fewer generic NTI drugs are on the market. Even though the market is huge, the barrier to entry is high. As of 2023, generic market share for NTI drugs is about 68%, compared to 90% for other drugs. Prescribers still hesitate. Patients worry. And manufacturers are cautious.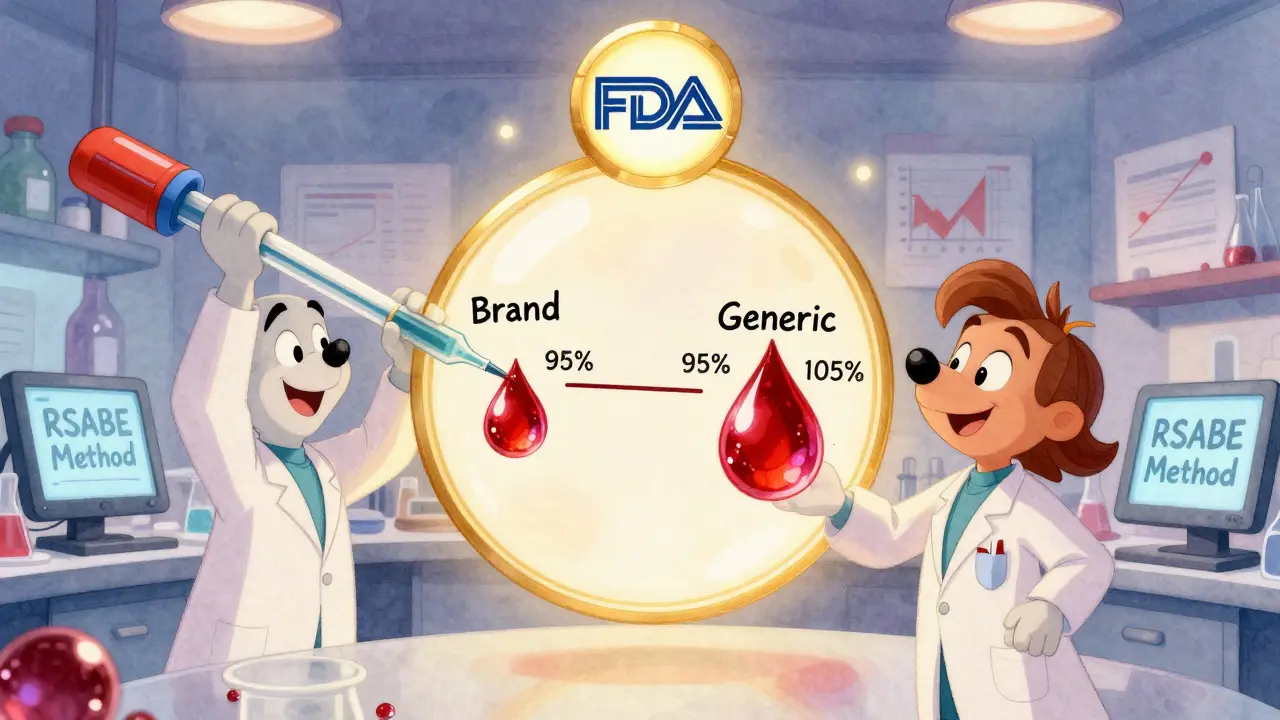
Real-World Evidence Shows Generics Can Be Safe - When They Meet the Standards
There’s a myth that generic NTI drugs are inherently riskier. That’s not true. The evidence says otherwise. A 2019 study in Circulation: Cardiovascular Quality and Outcomes followed over 2,000 patients on generic warfarin. No increase in clots or bleeding compared to the brand. Another study on levothyroxine found no difference in thyroid hormone levels or clinical outcomes between patients switched to generic versions - as long as the generic met the stricter bioequivalence criteria. The key word is “met.” Not all generics are equal. Only those that passed the FDA’s RSABE, variability check, and quality assay can be trusted. That’s why some generic versions of NTI drugs are approved, while others aren’t - even if they’re made by the same company. It’s not about the manufacturer. It’s about the data.What’s Changing in 2025?
The FDA doesn’t have a single official list of NTI drugs. They evaluate them case by case. That creates confusion. If you’re a pharmacist or a patient, how do you know if a generic is truly equivalent? In 2023, the FDA announced plans to create a more systematic way to classify NTI drugs using quantitative therapeutic index calculations - not just expert opinion. By mid-2024, they plan to release final guidance on RSABE for NTI drugs, making the process clearer for manufacturers. There’s also talk of global harmonization. The EMA, Health Canada, and the FDA are all moving toward tighter standards, but they’re not aligned. If they can agree on one set of rules - say, a hybrid of the FDA’s scaling and EMA’s fixed range - it could cut development costs by 15-20%. That might finally bring more affordable generics to market without sacrificing safety.
What This Means for Patients
If you’re on an NTI drug, you might wonder: Should I stick with the brand? Can I switch to generic? The answer depends on your doctor and your pharmacy. If your generic was approved under the FDA’s NTI bioequivalence criteria, it’s safe to use. But if you’re switching between different generic brands - even ones approved under the same rules - your doctor might still recommend monitoring your blood levels. Why? Because even small differences in how the drug is released in your gut can matter, especially with drugs like levothyroxine that are sensitive to food and timing. Bottom line: Don’t panic. Generic NTI drugs are safe when they meet the science-backed standards. But don’t assume all generics are the same. Talk to your pharmacist. Ask if the generic you’re getting passed the stricter NTI bioequivalence tests. And if you’re switched to a new generic, ask your doctor if a blood test is needed to confirm stability.Why This Matters Beyond the Pharmacy
This isn’t just about one class of drugs. It’s about how we balance access and safety in medicine. The FDA’s approach to NTI drugs shows that not all generics are created equal - and that’s okay. Rigorous standards aren’t a barrier to competition. They’re a way to ensure that when we say “generic,” we mean “safe and effective,” not just “cheaper.” As more NTI drugs come off patent, the pressure to make affordable alternatives will grow. But if we lower the bar, patients pay the price - in hospital visits, in complications, in lives. The current standards aren’t perfect. They’re expensive. They’re complex. But they’re built on real data, real outcomes, and real patient safety. The future of generic drugs isn’t about making them cheaper at all costs. It’s about making them trustworthy - especially when the stakes are highest.What drugs are considered narrow therapeutic index (NTI) drugs?
Common NTI drugs include warfarin, levothyroxine, digoxin, phenytoin, tacrolimus, sirolimus, lithium carbonate, theophylline, and carbamazepine. These drugs have a small margin between effective and toxic doses. The FDA doesn’t maintain a full public list but has issued specific bioequivalence guidance for 15 NTI drugs as of 2023, including those listed above.
Why are bioequivalence requirements stricter for NTI drugs?
Because even small changes in blood concentration - as little as 10% - can lead to treatment failure or serious side effects. For example, a slight drop in warfarin levels can cause a blood clot; a small increase can cause dangerous bleeding. Standard bioequivalence limits (80-125%) are too wide for these drugs. Stricter rules ensure generic versions behave nearly identically to the brand in the body.
How does the FDA’s approach differ from the EMA’s?
The FDA uses Reference-Scaled Average Bioequivalence (RSABE), which adjusts limits based on how much the brand drug varies in people’s blood. It also requires a variability comparison and unscaled bioequivalence within 80-125%. The EMA uses a fixed range of 90-111% for all NTI drugs, regardless of variability. The FDA’s method is more scientifically tailored but more complex and expensive to test.
Are generic NTI drugs safe to use?
Yes - if they’ve passed the stricter regulatory requirements. Real-world studies show no increase in adverse events when generic warfarin, levothyroxine, or tacrolimus meet FDA or EMA NTI bioequivalence standards. The risk comes from switching between different generic versions without monitoring, not from generics themselves.
Why are fewer generic NTI drugs available than regular generics?
Because NTI bioequivalence studies are more complex, require more participants, and cost $500,000-$1 million - nearly double the cost of standard generic studies. This higher barrier discourages manufacturers, even though the market is large. As a result, generic market share for NTI drugs is around 68%, compared to 90% for other drugs.
Should I avoid switching to a generic NTI drug?
Not necessarily. If your generic was approved under the FDA’s or EMA’s NTI guidelines, it’s safe. But if you’re switching between different generic brands - even ones approved under the same rules - your doctor may recommend checking your blood levels, especially for drugs like levothyroxine or warfarin. Consistency matters more than cost when the margin for error is tiny.


Lynsey Tyson
December 18, 2025 AT 13:04Just switched my mom to generic levothyroxine last year after her insurance dropped the brand. No issues at all. Her TSH stayed perfect. Honestly, if the FDA says it’s good enough, I trust them.
People freak out over nothing.
Edington Renwick
December 19, 2025 AT 11:32Let’s be real - this whole NTI thing is just Big Pharma’s way of keeping generics off the market. They don’t want competition. The ‘science’? Total theater. Same active ingredient. Same pill. Just a different label. If it works for the brand, it works for the generic. End of story.
Allison Pannabekcer
December 20, 2025 AT 13:17I work in a community pharmacy and I see this all the time. Patients panic when they get a different generic - even if it’s the same one they’ve been on for years, just a new batch from a different manufacturer.
Most of the time, it’s psychological. But sometimes? It’s real. That’s why we always check labs after a switch - especially with warfarin or lithium.
The FDA’s rules aren’t perfect, but they’re the best we’ve got. And honestly? I’d rather pay a little more for a generic that’s been rigorously tested than risk a hospital stay because someone cut corners.
It’s not about fear. It’s about responsibility.
Also - if your doctor doesn’t monitor you on these meds, find a new one. Period.
Sarah McQuillan
December 21, 2025 AT 19:52USA only. That’s the only reason this is even a thing. Europe? They’ve been doing this for decades. Canada? Same. But here? We’re stuck in some bureaucratic nightmare because ‘we’re special’.
Meanwhile, India and China make these generics cheaper and better. Why can’t we just import them? Oh right - because Big Pharma owns Congress.
Aboobakar Muhammedali
December 22, 2025 AT 00:40in india we dont have this problem because we dont have big pharma controlling everything
we just make the medicine and people take it
if it works its good if it dont its bad
no 500k studies no 36 person trials
just medicine
and people live
no drama
just life
anthony funes gomez
December 22, 2025 AT 22:01RSABE is statistically elegant - it’s a Bayesian adaptive approach that accounts for intra-subject variability in the reference product, thereby reducing Type I error inflation while maintaining power - but the regulatory implementation is unnecessarily convoluted, and the requirement for fully replicated crossover designs is economically inefficient, especially when considering the pharmacokinetic homogeneity observed in many NTI drugs across diverse populations - not to mention the ethical implications of exposing healthy volunteers to repeated dosing in high-risk pharmacodynamic contexts.
Laura Hamill
December 23, 2025 AT 17:14THEY’RE LYING TO YOU. The FDA doesn’t want you to know this - but the ‘strict standards’? They’re a cover. The real reason generics are so expensive to make? Because the same companies that make the brand drugs ALSO make the generics. Same factory. Same machines. Same chemists. They just change the label. You’re paying extra for a lie. 💔
Wake up. This isn’t safety. It’s profit.
Alana Koerts
December 25, 2025 AT 14:15So what? The study you cited had 2000 patients. Big deal. What about the 12 patients who had bleeding events? Did they get compensated? No. Did the FDA apologize? No. So don’t act like this is some moral victory. It’s just corporate risk management dressed up as science.
pascal pantel
December 26, 2025 AT 18:13Let’s cut through the noise. The FDA’s RSABE method is a mathematical sleight of hand. They allow wider margins for high-variability drugs - but who defines ‘high variability’? The brand manufacturer. That’s a conflict of interest. And the ‘quality assay’? A joke. They test one batch. One. That’s not science - that’s guesswork with a lab coat.
Gloria Parraz
December 27, 2025 AT 07:54For anyone scared to switch: talk to your pharmacist. They know which generics have passed the NTI criteria. Most of them can pull up the FDA’s database in seconds.
And if your doctor is nervous about switching? Ask them why. If they say ‘I don’t know’ - that’s not a reason to stay on the brand. It’s a reason to find a doctor who actually understands the data.
You’re not being reckless if you switch - you’re being smart. Just be informed.
Sahil jassy
December 28, 2025 AT 11:45bro in india we use generic tacrolimus for transplant patients and no one dies
we dont even have blood test every week
they just give the pill and go
if you feel bad you go to doctor
simple
why usa make it so hard
just give the medicine
people are not fragile
Nicole Rutherford
December 30, 2025 AT 03:18Oh please. You think this is about safety? It’s about control. Who gets to prescribe? Who gets to monitor? Who gets to decide what ‘safe’ means? It’s not the patient. It’s the system. And the system doesn’t want you to be independent. It wants you dependent. On the brand. On the doctor. On the lab. On the $800 monthly copay.
They’re not protecting you. They’re profiting from your fear.
Mark Able
December 31, 2025 AT 17:26Hey I’m a nurse. I’ve seen patients switch from brand to generic and have zero issues. But I’ve also seen people switch between two different generics and get confused - like they think the pill color change means it’s a different drug.
So here’s my advice: if you’re on an NTI drug, don’t switch unless you have to. And if you do? Take a picture of the pill. Write down the name. And tell your pharmacist you’re paranoid - they’ll love you for it.
Lynsey Tyson
January 2, 2026 AT 07:21That’s why I always ask for the same generic manufacturer. If my pharmacy switches it without telling me? I go back and ask why. It’s not about brand loyalty - it’s about consistency. My mom’s thyroid doesn’t care who made it. But it does care if the dose changes by 5%.