Glaucoma IOP Reduction Calculator
Calculate IOP Reduction
When people talk about Medical marijuana is a cannabis‑derived product used for therapeutic purposes, containing cannabinoids like THC and CBD, they often wonder if it can help eye health. The phrase medical marijuana glaucoma captures the core of this debate.
Key Takeaways
- THC can lower intraocular pressure (IOP) but the effect lasts only 3‑4 hours.
- CBD shows little to no IOP‑lowering benefit and may even raise pressure in some studies.
- Smoking or vaping marijuana delivers the fastest IOP drop, while edibles and tinctures act more slowly.
- Standard glaucoma drops (prostaglandin analogs, beta‑blockers) provide consistent 20‑30% pressure reduction around the clock.
- Legal, dosage, and side‑effect considerations make medical marijuana a supplemental option, not a first‑line therapy.
Understanding Glaucoma and Intraocular Pressure
Glaucoma is a group of eye diseases that damage the optic nerve, often linked to elevated intraocular pressure (IOP). If untreated, the pressure can erode the optic nerve fibers, leading to irreversible vision loss.
The key metric doctors monitor is Intraocular Pressure (IOP), the fluid pressure inside the eye, measured in millimeters of mercury (mmHg). Normal IOP ranges from 10‑21mmHg. Most glaucoma therapies aim to keep IOP below 18mmHg to slow disease progression.
How Cannabis Compounds Interact with Eye Pressure
Two main cannabinoids are discussed in eye‑health research:
THC (tetrahydrocannabinol) is the psychoactive component of cannabis that binds to CB1 receptors in the brain and eye. Early animal studies showed a 30‑40% IOP drop after smoking THC‑rich marijuana.
CBD (cannabidiol) is a non‑psychoactive cannabinoid that interacts weakly with eye‑specific receptors. Human trials generally report no significant IOP change, and some suggest a slight increase.
The mechanism is thought to involve cannabinoid receptors located in the ciliary body, the part of the eye that produces aqueous humor. Activating CB1 receptors reduces fluid production, temporarily lowering pressure.
Pros: What Medical Marijuana Can Do for Glaucoma
- Rapid IOP reduction - Smoking or vaporizing THC can lower pressure within minutes.
- Potential pain relief for patients with ocular discomfort or migraine‑type headaches.
- May be attractive for patients who dislike daily eye‑drop regimens.
- Some patients report improved overall well‑being, which can aid adherence to other glaucoma treatments.
Cons: Why Medical Marijuana Isn’t a Stand‑Alone Solution
- Short duration - The pressure‑lowering effect fades after 3‑4hours, requiring frequent dosing.
- Repeated dosing can lead to tolerance, diminishing effectiveness over time.
- Smoking introduces lung irritation and secondhand exposure concerns.
- THC’s psychoactive effects may impair driving, work performance, or cause anxiety.
- Legal restrictions vary; in many regions, medical cannabis is only available through licensed programs.
- Evidence is limited: most studies are small, short‑term, and often funded by non‑clinical sources.
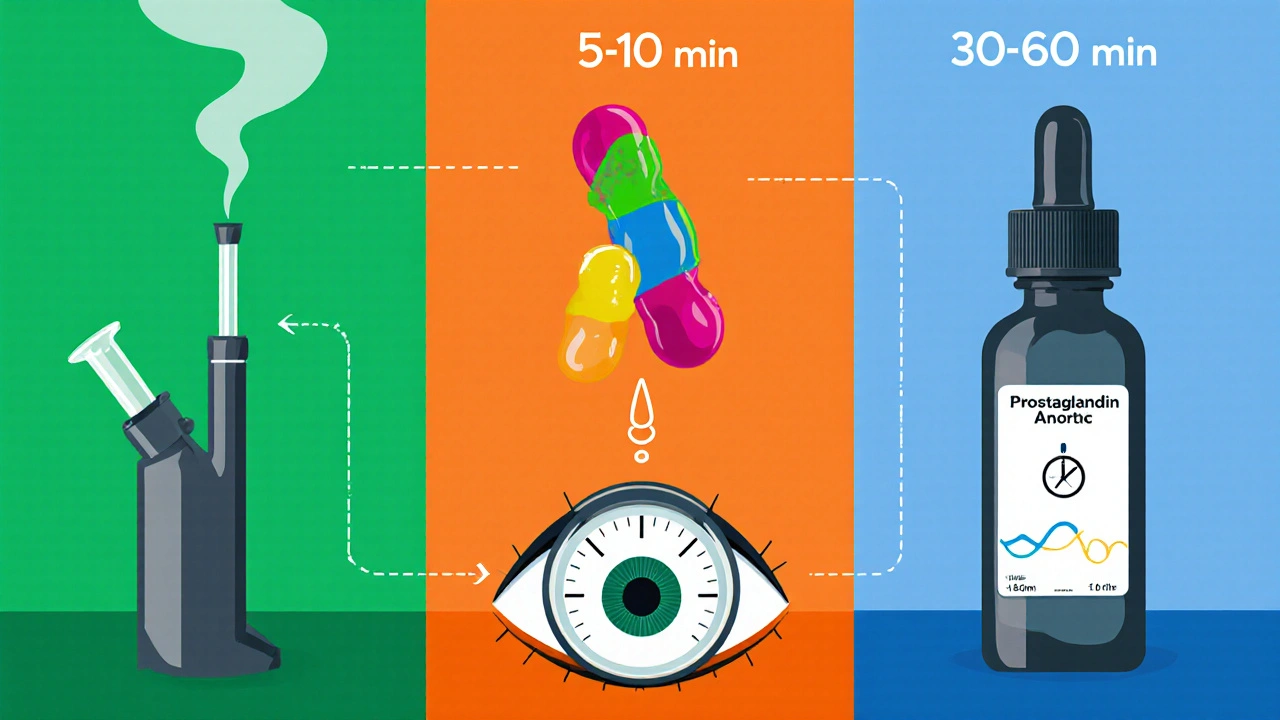
Comparing Delivery Methods
| Method | Onset | Duration | Typical IOP Reduction | Key Side Effects | Practical Considerations |
|---|---|---|---|---|---|
| Smoked/Vaped THC | 5‑10min | 3‑4hr | 25‑35% | Dry mouth, dizziness, psychoactive “high” | Frequent dosing needed; smoking not ideal for lung health |
| Oral THC (edible/tincture) | 30‑60min | 4‑6hr | 20‑30% | Gastro‑intestional upset, prolonged psychoactivity | Harder to dose precisely; delayed onset can be confusing |
| Topical CBD (experimental) | 15‑30min | 2‑3hr | ~0% (no proven IOP effect) | Skin irritation, rare allergic reaction | Easy to apply, but lacks pressure‑lowering benefit |
| Prostaglandin analog eye drops | 1‑2hr | 24hr | 20‑30% | Eye redness, increased eyelash growth | Once‑daily dosing; requires consistent administration |
| Beta‑blocker eye drops | 30‑60min | 12‑24hr | 15‑25% | Dry eyes, potential heart rate changes | Twice‑daily dosing; contraindicated in asthma or heart block |
Legal Landscape in Australia (and What It Means for You)
In Australia, medical cannabis is legal under strict prescription pathways. The Therapeutic Goods Administration (TGA) permits products containing THC, CBD, or both when a specialist authorizes them. However, the supply chain is tightly controlled: patients must obtain a prescription, then purchase from an approved pharmacy or licensed supplier.
Because glaucoma is a chronic condition, doctors often prefer tried‑and‑tested eye drops over cannabis, unless other therapies have failed or the patient has a compelling reason to try an alternative.

Practical Tips If You Choose to Explore Cannabis for Glaucoma
- Consult a qualified ophthalmologist first. They can document baseline IOP and visual field status.
- Get a medical cannabis prescription from a specialist who is familiar with ocular applications.
- Start with a low‑dose THC product (e.g., 2.5mg) and monitor IOP at 30min, 1hr, and 3hr after use.
- Record any side effects-especially dizziness, mood changes, or visual disturbances.
- Maintain your standard eye‑drop regimen unless your doctor advises otherwise.
- Schedule regular follow‑ups every 3‑6months to assess disease progression.
When Medical Marijuana May Be Considered
Patients who:
- Have progressed despite maximum tolerated conventional therapy.
- Experience severe side effects from beta‑blockers or prostaglandin analogs.
- Are already using cannabis for other medical reasons and can safely monitor IOP.
Even in these scenarios, cannabis should be viewed as an adjunct, not a replacement.
Frequently Asked Questions
Does marijuana actually lower eye pressure?
Yes, THC can drop IOP by about 25‑35% within minutes, but the effect usually wears off after 3‑4hours, making it impractical as a sole treatment.
How long does the pressure‑lowering effect last?
Typically 3‑4hours for smoked or vaporized THC. Oral forms may stretch to 4‑6hours, but the reduction is less consistent.
Is smoking weed safe for my eyes?
Smoking introduces harmful particulates that can irritate the eyes and lungs. Vaporizing reduces lung exposure but still delivers THC’s psychoactive effects, which may be undesirable for many patients.
Can CBD help with glaucoma?
Current research shows CBD does not significantly lower IOP and may even raise pressure in some cases. It is not recommended as a primary glaucoma therapy.
What are the legal ways to obtain medical marijuana for glaucoma in Australia?
You need a specialist’s prescription, after which a licensed pharmacy or approved supplier can dispense a TGA‑approved cannabis product. Recreational purchase remains illegal.
Are there long‑term risks of using cannabis for eye pressure?
Long‑term, frequent THC use can lead to tolerance, dependence, and potential cardiovascular effects. There is no evidence it damages the optic nerve, but the lack of sustained IOP control poses a risk of disease progression.
How does cannabis compare to prescription eye drops?
Eye drops provide consistent, around‑the‑clock IOP reduction with well‑documented safety profiles. Cannabis offers a rapid but fleeting drop, accompanied by systemic side effects, making it a supplemental rather than primary option.
Bottom Line
Medical marijuana can temporarily lower eye pressure, but its short action, psychoactive effects, and legal hurdles limit its usefulness as a standalone glaucoma treatment. For most patients, established eye‑drop medications remain the safest, most reliable choice. If you’re curious about cannabis, discuss it with your eye doctor, start low, and keep close tabs on your pressure readings.


Nikita Warner
October 12, 2025 AT 03:28When a patient with primary open‑angle glaucoma asks whether THC could replace prostaglandin analogs, the clinician must first outline the pharmacodynamic profile of cannabinoids in the eye.
Studies from the 1970s demonstrated that inhaled THC can achieve a 25‑35 % reduction in intraocular pressure within ten minutes of administration.
This rapid onset is attributable to the activation of CB1 receptors in the ciliary body, which transiently suppress aqueous humor production.
However, the same receptor desensitization occurs within three to four hours, necessitating repeated dosing to maintain therapeutic effect.
Repeated dosing, in turn, raises the risk of tolerance, meaning subsequent administrations yield diminishing pressure‑lowering returns.
Moreover, the systemic psychoactive burden of THC-including dizziness, dry mouth, and impaired psychomotor function-poses safety concerns for patients who must drive or operate machinery.
Oral formulations such as tinctures or edibles provide a more gradual absorption curve, extending the effect to four‑six hours, but they also introduce variability in bioavailability that can confound precise IOP monitoring.
From a regulatory standpoint, most jurisdictions, including Australia, restrict medical cannabis to specialist‑prescribed products, limiting accessibility for the average glaucoma patient.
The legal pathway typically requires a documented failure of conventional therapy, a thorough ophthalmologic assessment, and a signed treatment plan outlining dosage and monitoring frequency.
Practically, any patient electing to trial cannabis should establish a baseline IOP measurement, then record pressures at thirty‑minute, one‑hour, and three‑hour intervals after each dose.
This data‑driven approach enables the ophthalmologist to quantify the magnitude and duration of pressure reduction, as well as to detect any paradoxical pressure spikes.
In parallel, clinicians must counsel patients on potential cardiovascular effects of chronic THC exposure, such as tachycardia or blood pressure fluctuations, which may be contraindicated in certain comorbidities.
Importantly, while cannabinoids may serve as an adjunctive therapy, they should never replace first‑line agents like prostaglandin analogs or beta‑blocker drops that provide proven 24‑hour control.
The consensus among peer‑reviewed ophthalmology societies remains that cannabis‑derived products are experimental and lack the robust longitudinal data required for guideline endorsement.
Therefore, the prudent clinical pathway is to continue standard eye‑drop therapy, integrate cannabis only after documented refractory disease, and maintain vigilant IOP surveillance.
Ultimately, the decision rests on a balanced risk‑benefit analysis, thorough patient education, and close collaboration with a board‑certified ophthalmologist.
Liam Mahoney
October 18, 2025 AT 03:28Yo, using weed for eye pressure is just a whack fad, not science.
Justin Ornellas
October 24, 2025 AT 03:28When you state that THC "lowers pressure" you must also note the precise magnitude-typically 25‑35 %-and that the effect wanes after merely three to four hours.
Neglecting to mention the ensuing tolerance risk misleads readers about long‑term efficacy.
Furthermore, the phrase "medical marijuana" should be capitalised consistently to avoid ambiguity with recreational use.
Precision in terminology upholds the scientific integrity of the discussion.
Eric Appiah Tano
October 30, 2025 AT 02:28I appreciate the detailed correction above; clarity is essential when patients are weighing treatment options.
By emphasizing both the quantitative IOP drop and the short duration, you give a realistic framework for shared decision‑making.
Encouraging patients to keep a log of their pressures will empower them to see the actual benefit, if any.
Let’s continue to stress that any cannabis trial should be adjunctive, never a replacement for proven eye‑drops.
Jonathan Lindsey
November 5, 2025 AT 02:28Ah, the ever‑fascinating notion that a plant can substitute for a bottle of prostaglandin-how delightfully naïve.
One must consider that the pharmacokinetics of smoked THC evaporate faster than a gossip rumor at a family reunion, rendering it utterly impractical for chronic disease management.
Moreover, the psychosomatic side‑effects, such as the dreaded "high," could jeopardize activities requiring vigilance, a fact often glossed over by optimistic proponents.
In contrast, beta‑blocker drops, though less glamorous, provide a dependable twenty‑plus percent reduction around the clock, without the need for frequent re‑dosing or legal hurdles.
Thus, while the curiosity is commendable, the pragmatic clinician will prioritize evidence‑backed regimens over experimental horticulture.
Gary Giang
November 11, 2025 AT 02:28Think of THC like a fireworks show: bright, impressive, but fleeting.
The eye‑drop regimen is more like a steady lantern, guiding you safely through the night.
If you enjoy the sparkle, ensure you have a reliable baseline to compare, otherwise you might be chasing shadows.
steve wowiling
November 17, 2025 AT 02:28Honestly, if I wanted a roller‑coaster, I’d ride a theme park, not rely on my vision meds.
Smoking weed for glaucoma feels like using a band‑aid to fix a broken bridge-dramatic but ultimately useless.
Warren Workman
November 23, 2025 AT 02:28From a contrarian perspective, the paucity of long‑term RCT data renders any endorsement of cannabinoids for glaucoma scientifically untenable.
Moreover, the pharmacodynamic variability across strains introduces a jittery pharmacovigilance landscape that regulatory bodies are reluctant to endorse.
Consequently, the risk‑benefit calculus tilts heavily toward established prostaglandin analogs, whose mechanistic pathways are well‑characterized.
Shelby Rock
November 29, 2025 AT 02:28i reckon the eye is kinda like a window, u cant just slam it shut with weed and expect it to stay clear forever.
the mind can see beyond the pressure, but the optic nerve still feels the strain if you dont keep up the drops.
Alex Iosa
December 5, 2025 AT 02:28While the mainstream narrative paints medical cannabis as a benign adjunct, one must remain vigilant about hidden agendas.
Pharmaceutical conglomerates have vested interests in discrediting alternative therapies, yet they also stand to profit from the burgeoning market of proprietary cannabinoid extracts.
The paradox underscores the necessity for independent research, free from corporate patronage.
melissa hird
December 11, 2025 AT 02:28Oh, splendid-another “miracle cure” that promises to melt away eye pressure like butter on toast.
As if we needed more buzzwords in the medical lexicon.
Abraham Gayah
December 17, 2025 AT 02:28Well, if you’re looking for a drama‑filled adventure, lighting up a joint before your ophthalmology appointment certainly qualifies.
Just don’t be surprised when the IOP numbers swing like a theatre curtain and you end up with a plot twist of vision loss.
rajendra kanoujiya
December 23, 2025 AT 02:28Contrary to the hype, the fleeting IOP dip from THC is about as reliable as a weather forecast from a fortune‑cookie.
Caley Ross
December 29, 2025 AT 02:28From a chill observer’s standpoint, the data shows THC works, but only for a short burst-so if you’re okay with that limitation, it could fit your routine.
Craig Stephenson
January 4, 2026 AT 02:28Stay on track with your eye‑drops, but if you want to try cannabis, just keep a simple log and talk to your doctor.
John Nix
January 10, 2026 AT 02:28In accordance with current ophthalmic guidelines, medical cannabis should be considered solely as an adjunct after thorough evaluation of risk versus benefit.
Mike Rylance
January 16, 2026 AT 02:28Remember, consistent monitoring and open dialogue with your specialist are the pillars of successful glaucoma management, regardless of supplemental therapies.
Becky B
January 22, 2026 AT 02:28Some whisper that the pharmaceutical elite suppresses cannabis research to protect their profit margins, a claim that fuels distrust yet underscores the importance of independent validation.