When your body’s own immune system is turned against cancer, something powerful happens. For decades, doctors treated cancer with surgery, radiation, and chemotherapy - all aimed at killing fast-growing cells. But those methods often hurt healthy tissue too. Now, a new wave of treatments is changing the game: immunotherapy. Two of the most promising approaches are checkpoint inhibitors and CAR-T cell therapy. They don’t poison cancer. They wake up your immune system to find and destroy it.
How Checkpoint Inhibitors Unleash the Immune System
Your immune system has built-in brakes. These are called checkpoints - proteins like PD-1 and CTLA-4 that keep T cells from attacking too hard and damaging healthy organs. Cancer cells exploit this. They turn on PD-L1, a protein that latches onto PD-1 on T cells and says, “Don’t attack me.” It’s like putting a stop sign on your body’s soldiers. Checkpoint inhibitors are monoclonal antibodies designed to block those stop signs. Drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) block PD-1. Ipilimumab (Yervoy) blocks CTLA-4. Once those brakes are released, T cells can see the cancer again and start killing it. These drugs work best in cancers with high mutation rates - like melanoma, lung cancer, and kidney cancer - because more mutations mean more visible targets for the immune system. In melanoma, about 40% of patients respond to anti-PD-1 therapy. Some stay in remission for years. That’s rare with older treatments. But it’s not magic. Only 20-40% of patients respond at all. And when it doesn’t work, it’s often because the tumor doesn’t have enough T cells inside it to begin with. No soldiers, no fight.What CAR-T Cell Therapy Is - And How It’s Made
CAR-T therapy is like giving your immune system a custom-made weapon. It starts with a simple blood draw. Your T cells are pulled out, sent to a lab, and genetically rewired to carry a synthetic receptor called a chimeric antigen receptor (CAR). This CAR is designed to lock onto a specific protein on cancer cells - usually CD19 in blood cancers like leukemia and lymphoma. The modified T cells are grown in huge numbers - billions of them - then put back into your body. Before that, you get chemotherapy to clear out your existing immune cells. This makes room for the new ones. Within weeks, these engineered soldiers flood your bloodstream, hunt down cancer, and multiply as they go. The results are dramatic. In children with relapsed acute lymphoblastic leukemia (ALL), complete response rates hit 80-90%. Some who had no other options are now cancer-free five years later. For certain types of non-Hodgkin lymphoma, CAR-T therapy works even after multiple rounds of chemo failed. But this isn’t a pill you pick up at the pharmacy. It’s a personalized treatment. Each batch is made for one person. The whole process - from blood draw to reinfusion - takes 3 to 5 weeks. That delay can be deadly for someone whose cancer is growing fast.Why CAR-T Struggles with Solid Tumors
CAR-T therapy shines in blood cancers because the targets are easy to reach. But solid tumors - like lung, breast, or pancreatic cancer - are different. They’re surrounded by a fortress: scar tissue, suppressive immune cells, and chemicals that shut down T cells. Even if CAR-T cells make it into the tumor, they often get tired. They stop multiplying. They stop killing. The tumor microenvironment is like a wall of noise, drowning out the signal to attack. So far, CAR-T has shown less than 10% effectiveness in most solid tumors. The targets themselves are also harder to find. CD19 exists only on B cells - so targeting it is safe. But many solid tumor proteins also appear on healthy tissues. Hit those, and you risk damaging your heart, lungs, or gut. That’s called “on-target, off-tumor” toxicity. One patient treated for ovarian cancer had severe lung damage because the CAR targeted a protein also found in lung tissue. It’s a major reason why CAR-T hasn’t broken through in solid cancers yet.
Side Effects: What You Need to Know
Both therapies can cause serious side effects - but they’re different. Checkpoint inhibitors trigger immune-related adverse events (irAEs). Your immune system, no longer held back, can start attacking your own organs. Common ones include:- Rash or itching (30-40% of patients)
- Colitis (inflammation of the colon, 10-15%)
- Hypothyroidism (5-10%), which can cause fatigue and weight gain
- Pneumonitis (lung inflammation, up to 5%)
The Future: Combining Both Therapies
The real breakthrough may come from putting these two tools together. Checkpoint inhibitors give the immune system a boost. CAR-T cells bring the firepower. But giving them as separate drugs doesn’t work well - the side effects pile up, and the drugs don’t always reach the same place at the same time. Scientists are now engineering smarter CAR-T cells that make their own checkpoint blockers. Imagine a CAR-T cell that doesn’t just attack cancer - but also releases a PD-1 inhibitor right where it’s needed. This keeps the immune boost local, avoiding the whole-body inflammation caused by IV drugs. In mouse studies, this approach cut immune pneumonitis by 42% and boosted tumor-killing by 37%. Human trials are starting in 2024. Early results show promise for lung and ovarian cancers - two solid tumors that have resisted every other treatment. Another idea: “armored” CAR-T cells that secrete IL-12, a cytokine that helps T cells survive longer inside tumors. Or “off-the-shelf” CAR-T cells made from donor T cells, so patients don’t wait weeks for treatment. Even the targets are evolving. Instead of just CD19, researchers are testing CARs for BCMA (in myeloma), HER2 (in breast cancer), and even new ones like CLDN18.2 (in stomach cancer). The goal is to find targets that are unique to cancer - or at least rare in healthy tissue.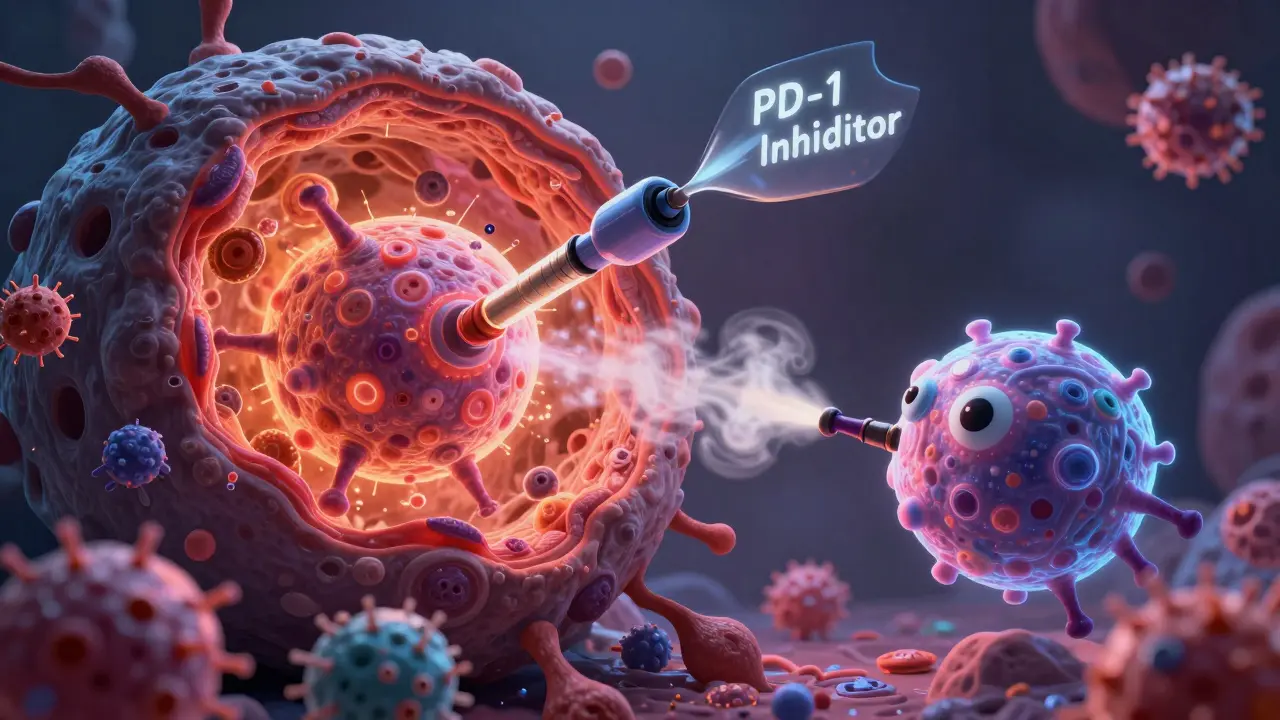


Carolyn Rose Meszaros
January 19, 2026 AT 11:55Emily Leigh
January 19, 2026 AT 22:37Greg Robertson
January 20, 2026 AT 19:29Crystal August
January 21, 2026 AT 03:39pragya mishra
January 22, 2026 AT 05:20Edith Brederode
January 23, 2026 AT 06:27Arlene Mathison
January 23, 2026 AT 16:09Renee Stringer
January 24, 2026 AT 18:46Manoj Kumar Billigunta
January 25, 2026 AT 21:49Andy Thompson
January 26, 2026 AT 14:34sagar sanadi
January 28, 2026 AT 06:52