When a doctor switches a patient from a brand-name drug to a generic, the patient often doesn’t get a new illness. They get the same active ingredient-same dose, same chemistry, same FDA-approved bioequivalence. But somehow, symptoms change. Fatigue sets in. Headaches appear. Anxiety spikes. And the patient blames the pill.
This isn’t a coincidence. It’s the nocebo effect in action.
The word comes from Latin: nocebo means “I shall harm.” Unlike the placebo effect-where positive expectations make a treatment work better-the nocebo effect is when negative expectations make things worse. Even if the pill is inert. Even if it’s chemically identical to what the patient took before.
A 2025 study tested this with sham oxytocin sprays. Healthy volunteers were told they were getting either a brand-name drug (simple name, high price) or a generic (complex name, low price). Both groups got nothing but saline. But those told they were getting the generic reported more side effects-and more of them. The difference wasn’t chemical. It was psychological. And it was statistically significant.
This isn’t rare. In the U.S., 90% of prescriptions are for generics. Yet nearly 4 in 10 patients still believe generics are less effective. When they switch, they start noticing every little ache, every mood swing, every sleepless night-and they link it to the new pill. It’s not that the drug changed. It’s that their brain did.
Why the Brain Believes the Generic Is Worse
Our brains are prediction machines. They don’t just react to what’s happening-they anticipate it. And if you’ve been told generics are “cheap,” “inferior,” or “not as good,” your brain starts scanning for signs that prove it right.
It’s not just about price. Packaging matters too. A 2024 study gave people a fake anti-itch cream. One group got it in a sleek blue box labeled Solestan® Creme. The other got the same cream in a plain orange box labeled Imotadil-LeniPharma Creme. Both had zero active ingredients. But the group with the expensive-looking box reported less pain sensitivity. The group with the generic-looking box reported more. Not because the cream worked differently. Because their brain expected it to hurt more.
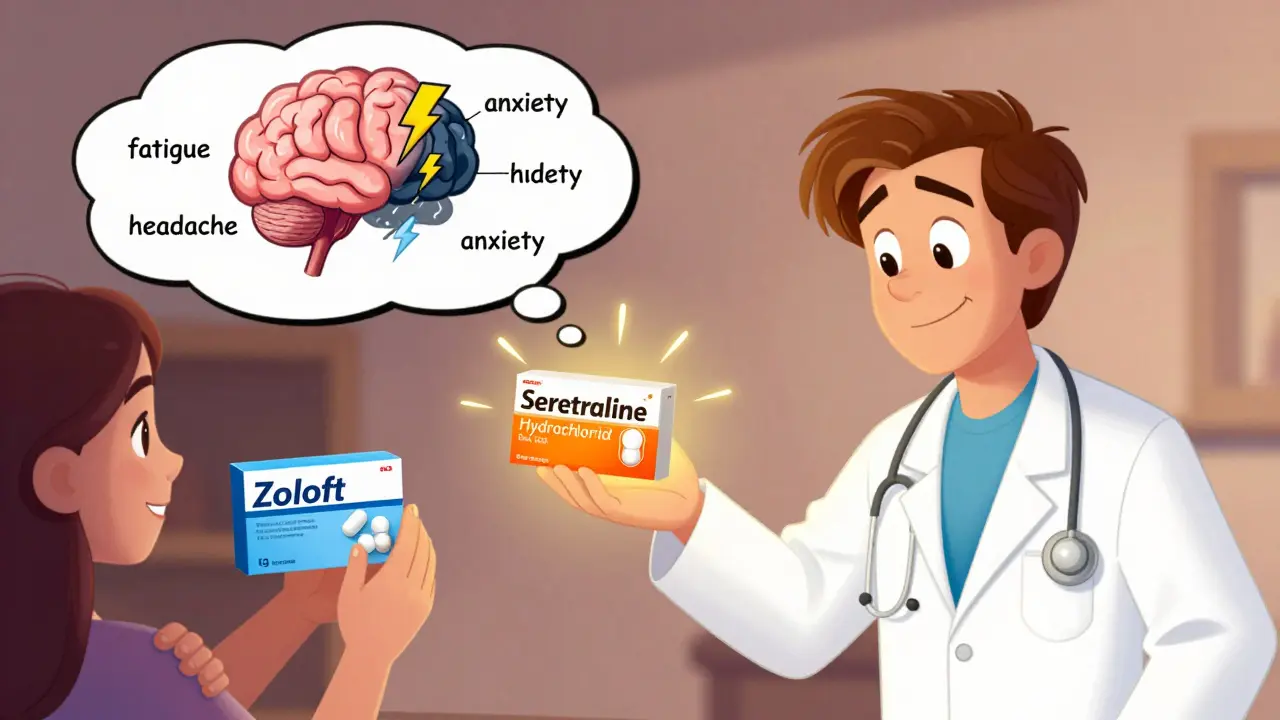
Even the name of the drug plays a role. A generic version of sertraline might be called “Sertraline Hydrochloride Tablets USP, 50 mg” by a manufacturer like “PharmaNova Inc.” That’s a mouthful. It sounds clinical. Unfamiliar. The brand version? Zoloft. Clean. Recognizable. Trusted. Your brain doesn’t care that they’re identical. It cares that one feels like a known quantity and the other feels like a gamble.
And when media stories pop up-“Generic Switch Caused My Depression to Return!”-it fuels the fear. One patient on Reddit wrote: “I was stable on Zoloft for 5 years. Switched to generic. Within days, I couldn’t get out of bed.” That story gets shared. It sticks. And the next person who switches? They’re already primed to feel worse.
What Bioequivalence Really Means
The FDA doesn’t just approve generics because they’re cheaper. They require proof that the generic delivers the same amount of active ingredient into the bloodstream at the same rate as the brand. That’s called bioequivalence. The acceptable range? The amount absorbed must fall within 80-125% of the brand’s levels. That’s not a loophole. That’s a tight, scientifically validated standard.
For most drugs, that range means no meaningful difference in effect. For drugs with narrow therapeutic windows-like warfarin or levothyroxine-doctors monitor levels closely regardless of brand or generic. But even there, studies show no consistent difference in outcomes between the two when properly managed.
Yet patients still report side effects after switching. Why? Because the body isn’t the problem. The expectation is.
A 2023 study in PLOS Medicine looked at authorized generics-medications made by the same company as the brand, in the same factory, with identical packaging except for the name. Patients still reported more side effects on the generic version. The drug didn’t change. The patient’s belief did.
How Healthcare Providers Can Reduce the Nocebo Effect
Doctors and pharmacists aren’t just prescribers. They’re expectation managers.
Here’s what works:
- Don’t lead with the word “generic.” Instead, say: “This is the same medicine you were taking, just without the brand name.”
- Reframe side effects positively. Don’t say: “Common side effects include dizziness, nausea, and fatigue.” Say: “Most people tolerate this well. If you feel a little tired at first, it usually passes in a few days.”
- Explain the cost savings. A 2022 study found that when patients were told switching to a generic could save them over $3,000 a year-*alongside* reassurance about effectiveness-nocebo effects dropped by 37%.
- Use trusted language. “This is the same medication approved by the FDA.” “Your insurance requires this version, but it’s just as safe and effective.”
- Don’t overwhelm with lists. Listing every possible side effect-even if it’s legally required-can prime patients to notice them. Focus on what’s common and temporary. Save rare risks for follow-ups.
Kaiser Permanente uses a simple script for switches: “This medication contains the exact same active ingredient as what you were taking before. Studies show patients do just as well on the generic version.” That’s it. No jargon. No fear. Just clarity.
When Patients Already Feel Worse After Switching
Some patients come in after a switch, convinced the generic is causing their symptoms. Their blood tests are normal. Their drug levels are identical. Their symptoms are real-but not caused by the medicine.
In these cases, dismissing their concerns makes things worse. Saying “It’s just in your head” triggers shame and distrust.
Instead, say: “I believe you’re feeling this. Let’s look at what might be going on.”
Then offer options:
- Return to the brand temporarily to confirm the effect.
- Wait 2-3 weeks. Many nocebo symptoms fade as expectations adjust.
- Try a different generic manufacturer. Some have different fillers or coatings that might affect tolerability-even if the active ingredient is the same.
- Use the Beliefs about Medicines Questionnaire (BMQ) to assess their level of concern about side effects and need for medication. This helps tailor the conversation.
One patient in Edinburgh switched from brand-name venlafaxine to a generic after her insurance changed. She reported panic attacks and insomnia. Her doctor didn’t argue. He said: “Let’s try going back to the brand for a month. If you feel better, we’ll know it’s not your condition returning. It’s your brain adjusting.” She did. She felt better. Then they switched back-with a detailed explanation about bioequivalence and a note that many patients feel this way temporarily. She stayed on the generic for a year after that.
What Patients Can Do to Protect Themselves
Patients aren’t powerless. Here’s what helps:
- Ask: “Is this the same medicine I was on?” If yes, remind yourself: the pill hasn’t changed. Your brain has.
- Track symptoms objectively. Use a simple journal: “Day 1: Headache. Day 3: Tired after lunch. Day 7: No change.” This helps separate real trends from emotional spikes.
- Don’t self-diagnose on Reddit. Online forums amplify fear. One bad story can feel like a pattern. Real data shows most people do fine on generics.
- Ask your pharmacist about the manufacturer. Some generic brands are more consistent than others. If you had a bad experience with one, ask for a different one next time.
- Give it time. The nocebo effect often peaks in the first week. Then it fades.

The Bigger Picture: Why This Matters
This isn’t just about pills. It’s about trust in the system.
When patients believe generics are inferior, they’re less likely to take them. That means higher costs for everyone. It means more brand-name prescriptions, more insurance denials, more people skipping doses because they can’t afford them.
And it means unnecessary suffering. People stop working. They cancel appointments. They worry they’re “broken” because a pill made them feel off-even though the pill is identical.
Health systems in Europe and the U.S. are starting to act. The European Medicines Agency now advises that generic packaging should avoid triggering alarm. Kaiser Permanente trains staff to use positive scripts. Some pharmacies now offer “branded generics”-same drug, same quality, but with cleaner, more familiar packaging to reduce perceptual shock.
A 2021 meta-analysis of 37 studies found that up to 22% of reported side effects after generic switches were likely due to perception-not pharmacology.
That’s not a small number. That’s millions of people experiencing real discomfort because of a label, a price tag, or a bad story they heard.
Changing that starts with one conversation. One clear explanation. One moment where a clinician says: “I know this feels different. But it’s not.”
What’s Next?
Research is moving fast. Scientists are using fMRI to see how the brain responds to brand vs. generic labels. Others are testing apps that deliver personalized, positive messaging when patients fill a generic prescription.
For now, the best tool we have is honest, calm, confident communication. Not marketing. Not fear. Not silence.
Patients don’t need to be convinced they’re wrong. They need to feel heard-and then shown the truth.
The medicine hasn’t changed. But how we talk about it? That can.

Neil Thorogood
January 26, 2026 AT 02:52Jessica Knuteson
January 28, 2026 AT 01:48Angie Thompson
January 28, 2026 AT 15:28rasna saha
January 30, 2026 AT 08:52Skye Kooyman
February 1, 2026 AT 04:55James Nicoll
February 2, 2026 AT 07:25Uche Okoro
February 2, 2026 AT 11:08bella nash
February 3, 2026 AT 10:27Ryan W
February 4, 2026 AT 07:31