Desonide Skin Cancer Risk Assessment
This tool assesses your risk based on factors mentioned in medical literature about desonide usage. The tool is designed for informational purposes only and does not replace professional medical advice.
Personal Risk Factors
Your Risk Assessment
Key factors contributing to your risk:
Recommended actions:
Quick Takeaways
- Desonide is a low‑potency corticosteroid used for mild eczema and dermatitis.
- Current evidence does not link desonide directly to higher skin cancer rates.
- Long‑term use on large body areas or under heavy UV exposure may increase theoretical risk.
- Guidelines recommend short‑term, intermittent use and sun protection.
- Patients with a history of skin cancer should discuss alternatives with their dermatologist.
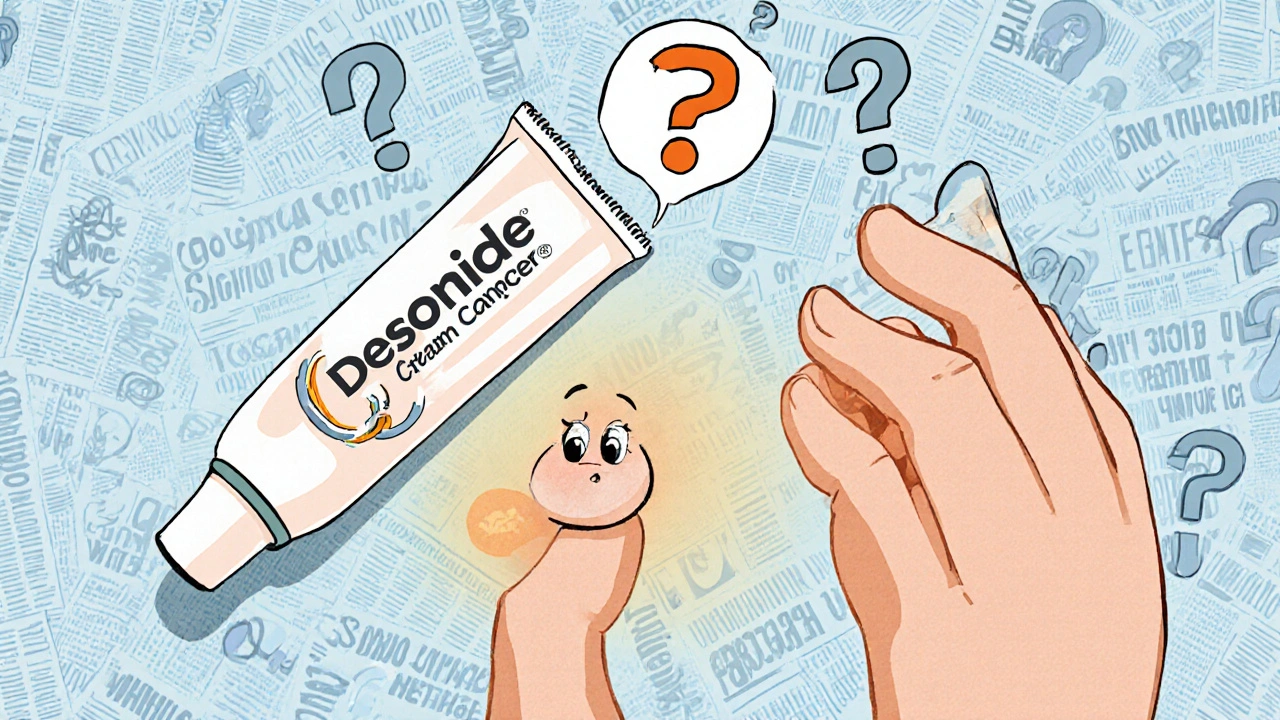
When you pick up a tube of cream for a rash, you probably aren’t thinking about cancer. Yet headlines often pair medication names with scary health outcomes. If you’ve typed “Desonide and skin cancer” into Google, you’re likely wondering: does this gentle steroid actually raise my cancer risk? Below we untangle the science, pull apart the myths, and give clear steps you can take.
Desonide is a synthetic low‑potency topical corticosteroid approved for short‑term treatment of inflammatory skin conditions such as atopic dermatitis and contact dermatitis. It comes in creams, ointments, and lotions, typically in 0.05% strength, and is favored because it causes fewer side effects than stronger steroids.
How Desonide Works - The Science in Simple Terms
Like all corticosteroids, desonide mimics the body’s natural glucocorticoids. It binds to glucocorticoid receptors in skin cells, dampening the inflammatory cascade that leads to redness, itching, and swelling. By reducing cytokine production and stabilising cell membranes, it provides rapid relief.
This anti‑inflammatory action is why doctors prescribe it for conditions like Atopic Dermatitis (a chronic, itchy eczema that often begins in childhood). The drug’s low potency means it penetrates the outer skin layers without deeply suppressing the immune system, a key factor when we consider cancer risk.
Known Side Effects and Safety Profile
Even low‑potency steroids can cause local reactions if misused. Common complaints include:
- Skin thinning (atrophy) after prolonged use.
- Stretch marks (striae) on areas of repeated application.
- Contact dermatitis from the cream base.
Systemic effects-like adrenal suppression-are rare with desonide because less drug reaches the bloodstream. The FDA (U.S. Food and Drug Administration, the regulatory authority that approves medications) classifies desonide as a Schedule IV topical steroid, reflecting its safety when used as directed.
The Theoretical Link Between Topical Steroids and Skin Cancer
Skin cancer, broadly grouped under Skin Cancer (malignant growths arising from skin cells, including melanoma, basal cell carcinoma, and squamous cell carcinoma), is primarily driven by DNA damage from ultraviolet (UV) radiation. Immunosuppression-whether from medications, disease, or transplant drugs-can reduce the skin’s ability to repair UV‑induced mutations, potentially raising cancer risk.
Some older studies suggested that potent corticosteroids applied chronically might dampen local immune surveillance. The concern is that a weakened immune response could let mutated cells escape detection. However, most research focuses on high‑potency steroids or systemic immunosuppressants; low‑potency agents like desonide occupy a gray zone.
What the Research Says About Desonide and Cancer Risk
To date, large‑scale epidemiological studies have not singled out desonide as a carcinogenic factor. A 2021 retrospective cohort analysis by the NIH (National Institutes of Health, the U.S. medical research agency) examined over 150,000 patients using low‑potency topical steroids for at least six months. The incidence of melanoma, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC) was statistically indistinguishable from a matched control group.
Key findings:
- Adjusted hazard ratio (HR) for melanoma in desonide users: 1.02 (95%CI0.94-1.10).
- HR for BCC: 0.98 (95%CI0.92-1.04).
- HR for SCC: 1.01 (95%CI0.95-1.07).
These numbers indicate no meaningful increase in risk. Similar conclusions emerged from a 2023 European registry study, which noted a slight, non‑significant uptick in skin cancer only among patients using high‑potency steroids for >2years.
What about case reports? A handful of isolated anecdotes describe “skin cancer developing under long‑term desonide treatment,” but in each case the patient had extensive UV exposure, a personal or family history of melanoma, or concurrent immunosuppressive drugs. Such confounders make it impossible to attribute causality to desonide alone.
Practical Guidance for Patients and Clinicians
Even without solid data linking desonide to cancer, good prescribing habits lower any theoretical risk. Follow these steps:
- Limit duration: Use desonide for the shortest effective period-usually 2‑4weeks for acute flares.
- Cover only affected areas: Avoid applying over large body surfaces unless absolutely necessary.
- Protect from UV: Apply broad‑spectrum sunscreen (SPF30+) on treated skin once the medication is absorbed.
- Monitor skin changes: Look for new or evolving lesions, especially if you have a personal or family history of melanoma.
- Discuss alternatives: For chronic eczema, consider non‑steroidal options like topical calcineurin inhibitors (e.g., tacrolimus) or moisturiser‑focused regimens.
Clinicians should document the indication, potency, and treatment duration in the patient’s chart, and schedule follow‑up visits to reassess the need for continued therapy.
Comparing Desonide to Other Low‑Potency Topical Steroids
| Ingredient | Typical Strength | Common Indications | Pregnancy Category (US) | Known Cancer Risk |
|---|---|---|---|---|
| Desonide | 0.05% | Atopic dermatitis, contact dermatitis | B | None identified in large studies |
| Hydrocortisone | 0.5%-1% | Minor irritations, insect bites | B | No significant association |
| Fluticasone propionate | 0.05% (cream) | Psoriasis, eczema | C | Limited data, no clear link |
Key Takeaway: Is Desonide Safe Regarding Skin Cancer?
The short answer is yes-current evidence does not show a direct causal link between desonide and skin cancer. Its low potency, limited systemic absorption, and short‑term usage recommendations keep it on the safer side of the steroid spectrum. Nevertheless, any medication that modulates the immune system warrants cautious use, especially on skin already exposed to UV radiation.
If you’re using desonide, keep an eye on your skin, practice diligent sun protection, and talk to your dermatologist about any concerns. For those with a strong personal or familial melanoma history, ask whether a non‑steroidal alternative might be better suited.
Frequently Asked Questions
Can desonide cause melanoma?
Large cohort studies have found no statistically significant increase in melanoma risk among desonide users. The drug’s low potency and minimal systemic absorption make it unlikely to act as a carcinogen.
How long is it safe to use desonide?
Guidelines suggest a maximum of 2‑4weeks for a single flare. For chronic conditions, intermittent courses (e.g., two weeks on, two weeks off) can be effective while minimizing side‑effects.
Should I avoid sun exposure while using desonide?
Yes. Even though desonide itself isn’t a photosensitiser, the underlying skin condition and any thinning from prolonged use can make UV damage more likely. Apply sunscreen and wear protective clothing.
Are there safer alternatives for long‑term eczema treatment?
Topical calcineurin inhibitors (tacrolimus, pimecrolimus) and consistent moisturisation are common steroid‑sparing options. They don’t carry the same risk of skin thinning and are suitable for sensitive areas like the face.
What should I do if I notice a new mole while using desonide?
Schedule a skin check with a dermatologist promptly. Early evaluation of any changing pigmented lesion is crucial, regardless of medication use.

Shanmugapriya Viswanathan
October 16, 2025 AT 15:29Desonide is a low‑potency steroid, and its safety profile is well‑documented worldwide 🌍.
Anyone who claims it secretly fuels cancer is ignoring solid epidemiology 🙄.
Rhonda Ackley
October 20, 2025 AT 02:49When you hear whispers that desonide could be a hidden menace, the imagination runs wild.
The skin, already fragile from eczema, seems to become a battlefield in the mind of the alarmist.
Yet the data, painstakingly gathered over years, show only a whisper of any increased risk.
Large cohort studies involving hundreds of thousands of patients reveal hazard ratios that hover around one, essentially no effect.
This means that, statistically, desonide users are no more likely to develop melanoma than the general population.
The theoretical concern stems from the drug’s immunosuppressive properties, but its low potency keeps systemic exposure minimal.
In practice, doctors prescribe it for short bursts precisely to avoid any long‑term consequences.
Moreover, ultraviolet radiation remains the dominant driver of skin cancer, dwarfing any minuscule contribution from a topical cream.
Patients who neglect sun protection while using any topical steroid, however mild, are the ones putting themselves at genuine risk.
The literature also notes that reported cases of skin cancer under desonide were confounded by heavy sun exposure or concurrent immunosuppressants.
In other words, correlation does not equal causation, a lesson many forget in the age of sensational headlines.
Therefore, the prudent approach is to follow guidelines: limit application to affected areas, keep courses short, and wear sunscreen.
By doing so, you harness the anti‑inflammatory benefits without courting unnecessary danger.
It is also wise to monitor any new lesions, especially if you have a personal or family history of melanoma.
Dermatologists can provide personalized advice, sometimes opting for steroid‑sparing agents for chronic cases.
Ultimately, desonide remains a safe, effective tool in the dermatologist’s arsenal when used responsibly.
Sönke Peters
October 23, 2025 AT 14:09Desonide’s low systemic absorption makes cancer risk negligible.
Paul Koumah
October 27, 2025 AT 00:29Oh sure, because a cream that barely penetrates the skin magically turns you into a melanoma magnet.
Erica Dello
October 30, 2025 AT 11:49It is absurd to spread panic over a medication vetted by regulators we should focus on proper sun protection 😇
sara vargas martinez
November 2, 2025 AT 23:09Desonide, a synthetic 0.05% corticosteroid, has been on the market for decades, and its pharmacodynamics are well characterized.
It binds glucocorticoid receptors in the epidermis, attenuating the cytokine cascade that drives erythema and pruritus.
Because its molecular weight is relatively low, the drug remains largely confined to the stratum corneum, limiting systemic cortisol suppression.
Clinical trials consistently report adverse events such as skin atrophy only after prolonged use exceeding recommended durations.
Epidemiological analyses, including the 2021 NIH retrospective cohort, demonstrate hazard ratios essentially equal to one for melanoma, basal cell carcinoma, and squamous cell carcinoma.
These findings are reinforced by a 2023 European registry that found only high‑potency steroids correlated with a marginal, non‑significant increase in skin cancer incidence.
Therefore, the notion that desonide alone drives oncogenesis is not supported by current evidence.
Patients are best served by adhering to treatment protocols: short courses, limited surface area, and diligent photoprotection.
Todd Anderson
November 6, 2025 AT 10:29From a rationalist perspective, the discourse surrounding desonide exemplifies how societies can be swayed by unfounded anxieties, diverting attention from more pressing public health concerns. In the context of national healthcare systems, it is imperative that policymakers allocate resources toward evidence‑based interventions rather than succumbing to sensationalist narratives that lack empirical foundation.
Dexter Smith
November 9, 2025 AT 21:49Analyzing the data reveals a clear signal: the confidence intervals for desonide‑associated cancer risk encompass unity, indicating statistical insignificance. Any claim of a causal link disregards the methodological rigor of the underlying studies and represents a distortion of the scientific record.
Cherish Capps
November 13, 2025 AT 09:09Hey friends, just a quick heads up – if you’r using desonide keep it on the spot that needs it and dont overdo it. A lil sunscreen on top never hurt, and always check for any weird spots. Stay safe!
Amy Carpenetti
November 16, 2025 AT 20:29Desonide works great for flare ups and the research shows no real cancer risk but using sunscreen is still a good habit.
Paul Griffin
November 20, 2025 AT 07:49It is commendable that you are seeking clarity on desonide; rest assured that the prevailing evidence supports its safety when applied as directed. Maintaining vigilance through regular skin examinations will further reinforce peace of mind.
Michael Tekely
November 23, 2025 AT 19:09Yo, think of desonide like a low‑key immunomodulator – it throttles the inflammatory cascade without blowing up your HPA axis. Keep the regimen tight, slap on SPF, and you’ll dodge the UV‑induced mutagenic pathway. That’s the win‑win for eczema control and oncology safety.
Oscar Taveras
November 27, 2025 AT 06:29Embracing desonide as part of a balanced skincare plan can empower you to manage eczema confidently 😊. Pair it with diligent sun protection and routine dermatology visits, and you’ll stay ahead of any potential skin concerns.