Drug Desensitization Eligibility Checker
This tool helps determine if drug desensitization might be appropriate for your situation based on clinical guidelines from the National Institutes of Health and Brigham and Women's Hospital.
Important: This is not a substitute for professional medical advice. Always consult an allergist or immunologist specializing in drug hypersensitivity.
When a life-saving medication triggers a dangerous allergic reaction, what do you do? Stop the treatment? Switch to something less effective? Or risk a reaction again? For many patients, there’s a third option: drug desensitization. It’s not a cure. It’s not a workaround. It’s a carefully controlled medical process that lets people safely receive drugs they’re allergic to-when no other choice exists.
What Exactly Is Drug Desensitization?
Drug desensitization is the process of gradually introducing a medication to someone who’s had a severe allergic reaction to it in the past. The goal isn’t to remove the allergy forever. It’s to temporarily turn off the body’s overactive response-just long enough to deliver the full dose needed to treat the illness. This isn’t magic. It’s science. The technique was developed in the 1960s at the National Institutes of Health and later refined by Dr. Mariana Castells and her team at Brigham and Women’s Hospital. Today, their protocol is the gold standard. It works by giving tiny, increasing doses of the drug over hours, not days. The immune system gets confused. It stops seeing the drug as a threat. And for that window of time, the patient can receive the full dose without a reaction. Success rates? Around 95% to 100% for immediate reactions like hives, swelling, or anaphylaxis. That’s not a guess. That’s from published clinical studies tracking thousands of patients. The catch? The tolerance disappears as soon as the drug is stopped. If you need it again next week? You go through the whole process again.When Is Desensitization Actually Needed?
You don’t do this just because you’re nervous about a reaction. You do it when the alternative is worse. The most common situations:- Antibiotics: You’re allergic to penicillin, but you have a severe bone infection (osteomyelitis) and only penicillin or a close cousin will kill the bacteria. Alternatives like vancomycin or clindamycin are less effective, harder to administer, or more likely to cause resistance.
- Chemotherapy: You have cancer. The best drug for your tumor type-like paclitaxel or carboplatin-is the one you reacted to. Skipping it means a lower chance of survival. Desensitization lets you get the most effective treatment.
- Monoclonal antibodies: Drugs like rituximab or trastuzumab are critical for autoimmune diseases or breast cancer. If you’ve had a reaction, and there’s no other option, desensitization is often the only way forward.
- Aspirin and NSAIDs: For people with asthma or nasal polyps who react to these drugs, a slow desensitization can restore tolerance and allow them to use them for pain or heart protection.
Two Types of Protocols: Fast and Slow
Not all reactions are the same. And not all desensitizations work the same way. Rapid Drug Desensitization (RDD) is used for immediate reactions-those that happen within minutes or an hour after exposure. Think hives, wheezing, low blood pressure. This is the most common type. The Brigham and Women’s Hospital protocol gives 12 doses over 4 to 6 hours. The first dose is 1/10,000th of the full dose. Each next dose doubles the previous one. Every 15 minutes, you get a little more. By the end of the day, you’ve received the full therapeutic dose. Patients are monitored continuously: blood pressure, oxygen levels, heart rate, breathing. Nurses watch for any sign of a reaction. If one happens, they stop, treat it, and then restart at a lower dose. Slow Drug Desensitization (SDD) is for delayed reactions-those that show up hours or days later. Think rash, fever, or organ inflammation. These are T-cell driven, not IgE-driven. There’s no standard protocol. Dosing intervals can be hours or even days apart. For aspirin, it might take 2 to 3 days to reach the full dose. Oral administration is common here. The process is slower, less intense, but still requires medical supervision. The route matters too. IV desensitization is most common for antibiotics and chemo (70% of cases). Oral is used for aspirin and NSAIDs. The timing between doses is stricter for oral-usually at least 60 minutes, sometimes longer.Why Not Just Pretreat With Antihistamines?
A lot of people think: “Why not just give me Benadryl and steroids before the drug and call it a day?” Because it doesn’t work well enough. Premedication reduces mild reactions. But when it comes to severe, life-threatening ones? It fails. In one study of 40 cancer patients getting paclitaxel, 4 out of 40 had serious reactions even after premedication. That’s a 10% failure rate. With desensitization? Less than 2% of patients have a severe reaction during the process-and almost all of those are manageable because they’re done in a controlled setting. Desensitization doesn’t just mask the reaction. It changes how the immune system responds to the drug. Premedication just dulls the symptoms. It doesn’t prevent the reaction from happening at its root.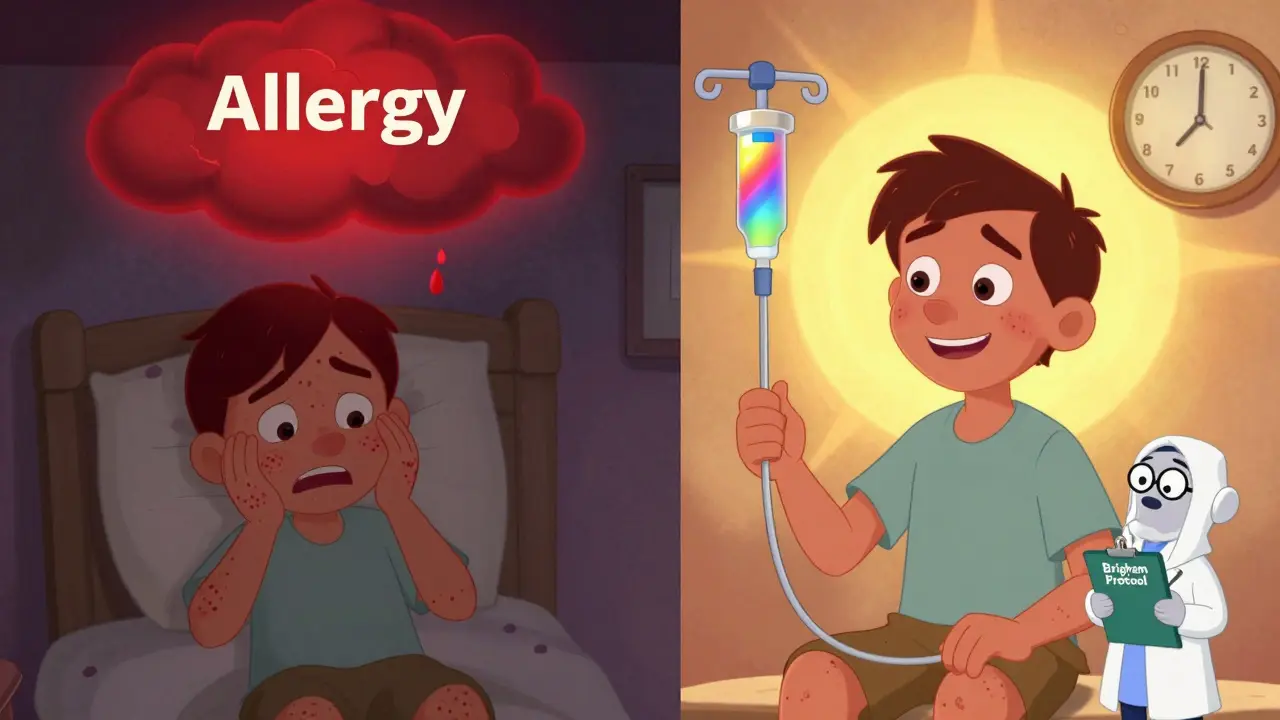
Who Should NOT Get Desensitization?
It’s not for everyone. And trying it on the wrong person can be deadly. Contraindications:- Severe delayed reactions like Stevens-Johnson syndrome or toxic epidermal necrolysis. These involve massive skin and organ damage. Desensitization won’t help-and could kill you.
- Patients with unstable heart or lung disease. The stress of the procedure can trigger complications.
- Patients who’ve had a reaction to the drug in the last 24 to 48 hours. The immune system is still primed. Too risky.
- Patients with a history of multiple drug allergies without clear triggers. The risk of cross-reactivity is too high.
What Happens During the Procedure?
You don’t just walk into a clinic and get started. It’s a hospital-based procedure. Here’s what it looks like:- You’re evaluated by an allergist or immunologist. They review your reaction history. They may do skin tests or blood tests to confirm the allergy type.
- They decide which protocol to use-rapid or slow-based on your reaction type and the drug.
- You’re admitted to a monitored unit. Usually an infusion center or ICU. Not a regular exam room.
- Nurses set up IV lines. Continuous monitors go on. Emergency meds (epinephrine, antihistamines, steroids) are ready.
- The first tiny dose is given. You wait 15 minutes. Vital signs checked.
- Dose doubles. Wait. Check.
- Repeat until full dose is reached.
- Once you’ve received the full dose, you’re monitored for at least another hour.
Success Stories and Real Risks
One patient, u/PenicillinWarrior on Reddit, spent 20 years avoiding penicillin because of a childhood rash. When he developed osteomyelitis, doctors said he’d need a 6-week IV antibiotic course. The only effective drug? Penicillin. He went through a 4-hour rapid desensitization. He completed the treatment. No reaction. He’s now back to work. In a 2022 study at Brigham and Women’s, 42 patients with penicillin allergies underwent rapid desensitization. Zero deaths. Zero anaphylactic events. Only 8% had mild symptoms-flushing, itching-that were easily treated. But here’s the flip side. A 2021 survey found that 12% of desensitization complications happened in community hospitals where staff weren’t trained. No proper dilution kits. No allergist on-site. No emergency equipment. The complication rate tripled. Desensitization isn’t risky because it’s dangerous. It’s risky because it’s done wrong.
Who Can Do It? And Where?
This isn’t something a general practitioner can handle. You need:- An allergist or immunologist with specialized training
- A team of nurses trained in anaphylaxis management
- A facility with emergency meds, monitors, and resuscitation equipment
- Standardized protocols-not a Google search
The Future: Smarter, Faster, Safer
Desensitization isn’t standing still. In 2023, the AAAAI released the first standardized national protocols, replacing 12 conflicting guidelines. That’s huge. New research is looking at biomarkers-like basophil activation tests-to predict who will respond to desensitization with 89% accuracy. Imagine knowing before you start whether it’ll work. Home-based desensitization is in phase 2 trials. For patients who’ve already been desensitized and need repeat treatments, a supervised home protocol could save time and money. Early results? 92% success. And the big picture? As antibiotic resistance climbs and cancer drugs get more complex, desensitization will become more common. The CDC reports 35,000 U.S. deaths annually from resistant infections. Many of those patients could be saved if they could safely use the most effective antibiotics. Dr. Castells says we’re heading toward precision desensitization-where genetic and immune profiles determine not just if you can be desensitized, but which protocol will work best for you.Bottom Line: It’s Not a Last Resort. It’s a Lifeline.
Drug desensitization isn’t a curiosity. It’s a proven, life-saving tool. It’s used when the stakes are highest: cancer, life-threatening infections, autoimmune disease. It’s not for every allergic reaction. It’s not for every drug. But when the right patient meets the right condition? It’s the only option that gives them a real chance. If you’ve been told you can’t take a critical medication because of an allergy, ask: Is desensitization an option? Don’t assume it’s too risky. Ask for a referral to an allergist who specializes in drug hypersensitivity. The right team, in the right setting, can make all the difference.For patients who’ve been through it, the message is clear: “I was allergic. Now I’m alive.”


Harsh Khandelwal
December 25, 2025 AT 10:12This whole desensitization thing is just Big Pharma’s way to hook you on drugs they know are toxic. They don’t want you to find alternatives-they want you addicted. I’ve seen the paperwork. The FDA approves these protocols because they’re paid off. You think they care if you live? Nah. They care if you keep coming back for more. And now they’re pushing home-based versions? Next thing you know, your grandma’s doing IV chemo in her living room while watching reruns of Wheel of Fortune.
Christine Détraz
December 25, 2025 AT 19:10I’ve seen this done in person. My cousin went through it for paclitaxel after her breast cancer diagnosis. She was terrified-but the nurses were so calm, so precise. She got through it with just a little flushing and some itching. No anaphylaxis. No ICU. Just a long, quiet 5 hours of being watched like a ticking clock. And now? She’s painting again. That’s the real win. Not the science. The art of being alive after it.
John Pearce CP
December 26, 2025 AT 00:49The notion that American medical institutions are somehow uniquely qualified to manage this procedure is laughable. In Germany, they have protocols refined over decades. In Japan, they use predictive biomarkers with 94% accuracy. Here? We’re still using 1980s-era dilution charts and hoping for the best. This isn’t innovation. It’s institutional laziness dressed up as progress. The U.S. doesn’t lead in medicine. It just spends the most money on it.
Isaac Bonillo Alcaina
December 26, 2025 AT 09:42You say success rates are 95-100%. That’s statistically misleading. You’re counting mild flushing as a success. A patient gets a rash, gets treated, and you call it a win? That’s not success. That’s triage. Real success is zero reactions. Full stop. And even then, the tolerance is temporary. You’re not curing anything. You’re buying time. And for what? To extend a life that may already be compromised by the disease you’re treating? It’s not heroic. It’s desperate.
Bhargav Patel
December 27, 2025 AT 00:46There is a profound metaphysical tension in this procedure. We are manipulating the immune system not to heal it, but to deceive it. We are asking the body to ignore a threat it has been evolutionarily wired to detect. In doing so, we are not merely treating disease-we are negotiating with biology on its own terms, and yet, we remain outsiders to its logic. Is this medicine? Or is it a temporary truce in an endless war? And if the truce ends when the drip stops, what have we truly achieved?
suhani mathur
December 27, 2025 AT 08:37Oh wow, so now we’re doing IV chemo like it’s a Starbucks latte? ‘Here’s your 1/10,000th dose, ma’am, would you like sugar with that anaphylaxis?’ Seriously, if your doctor suggests this and doesn’t have a board-certified allergist on standby, run. Not walk. Run. And tell them I sent you.
Diana Alime
December 28, 2025 AT 16:33ok so i read this whole thing and like… i cried? not because it’s sad but because i didn’t know this was even a thing. my aunt had to do this for her cancer and they just said ‘we’ll try it’ and she got through it. i thought it was just luck. turns out it’s science? that’s wild. i’m gonna send this to my cousin who’s allergic to penicillin and has pneumonia. maybe it’ll help. thank you??
Bartholomew Henry Allen
December 28, 2025 AT 17:44Desensitization is a luxury. It requires infrastructure. It requires trained personnel. It requires time. America cannot afford to give this to everyone. We should reserve it for those who have paid into the system. Not for undocumented immigrants. Not for the uninsured. Not for the lazy who refused to get tested. This is not a right. It is a privilege earned through responsibility.
Andrea Di Candia
December 30, 2025 AT 05:19I love how this isn’t just a medical procedure-it’s a story of human resilience. People who thought they’d never get to see their kids graduate, never get to travel again, never taste coffee without fear… they get to. And it’s not because of magic. It’s because of teams of people who showed up, day after day, to make sure someone else could live. That’s the real breakthrough. Not the science. The care.
bharath vinay
December 30, 2025 AT 08:11They say it’s 95% effective. But what about the 5%? Who’s counting them? The ones who went into the hospital alive and came out in a body bag? The ones whose families were told it was a ‘rare complication’? No one talks about them. Because if you admit the risk, you admit the lie. They’re not saving lives. They’re gambling with them. And the house always wins.
Dan Gaytan
December 31, 2025 AT 01:00Just had to say… this gave me chills. My brother did this for rituximab after his lupus flare. He was scared out of his mind. But the team held his hand through every step. Now he’s back hiking with his dog. I just wanted to say thank you for writing this. It’s not just info-it’s hope. 🙏❤️
Wilton Holliday
December 31, 2025 AT 07:23If you’re reading this and you’re scared because you’ve been told you can’t take a life-saving drug-please don’t give up. Ask for a referral. Find a specialist. This isn’t experimental. It’s routine in top hospitals. You’re not a risk. You’re a candidate. And there are people who’ve done this thousands of times. You’re not alone. I’ve walked patients through this. I’ve seen the tears. I’ve seen the relief. You’ve got this.