Contraceptive Guide for Endometriosis
Recommended Contraceptive Method
Important Note
This tool provides general guidance based on common considerations. Individual medical situations vary greatly. Always consult with a healthcare provider for personalized recommendations.
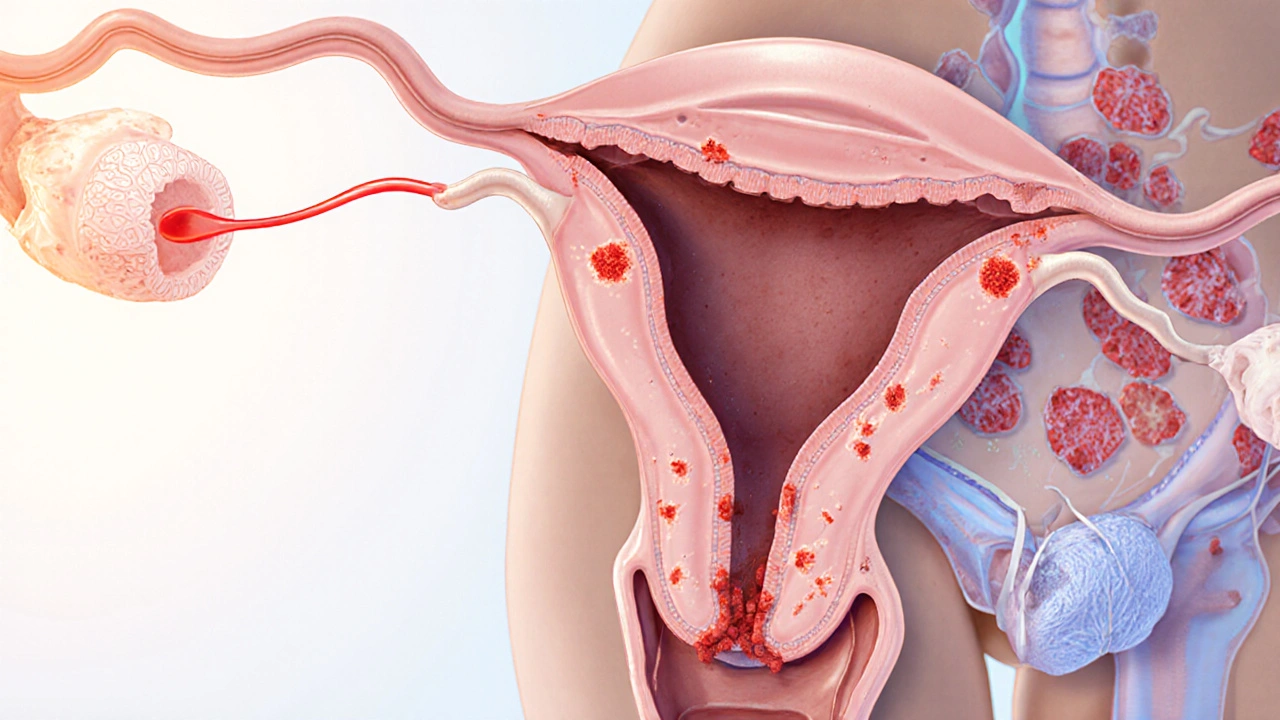
When talking about chronic pelvic pain, Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, causing inflammation, scar tissue, and often severe pain. The disease affects roughly 1 in 10 women of reproductive age and can dramatically affect quality of life. A frequent question on health forums is whether contraception can help prevent its onset or ease its symptoms. Below we break down the science, compare the most common birth‑control options, and give practical tips for anyone navigating both topics.
Key Takeaways
- Hormonal contraceptives that suppress ovulation-especially combined oral pills and progestin‑only methods-are the only birth‑control options proven to reduce endometriosis lesion growth.
- Long‑acting intrauterine devices (IUDs) work differently: a levonorgestrel IUD offers hormonal relief, while a copper IUD provides no hormonal benefit and may leave symptoms unchanged.
- Choosing a method depends on age, symptom severity, fertility plans, and personal tolerance for side effects.
- Non‑hormonal methods (condoms, diaphragms, copper IUD) do not address the disease mechanism, but they are safe for women who cannot take hormones.
- Regular follow‑up with a gynecologist is essential; medication adjustments often improve pain control and quality of life.
What Is Endometriosis and How Does It Develop?
Endometriosis originates from retrograde menstruation, where menstrual blood flows backward into the pelvic cavity. The displaced endometrial‑like cells implant on the ovaries, fallopian tubes, peritoneum, and sometimes distant organs. Over time, these implants respond to the menstrual cycle, bleeding each month, which triggers inflammation and scar tissue (adhesions). The main symptoms include:
- Pelvic or lower‑back pain, often worsening during periods.
- Painful intercourse (dyspareunia).
- Heavy or irregular bleeding.
- Infertility in up to 30‑40% of affected women.
Diagnosis typically involves a transvaginal ultrasound, MRI, and sometimes laparoscopic biopsy. Early detection matters because the disease can progress silently for years.
How Contraception Interacts With Endometriosis
Contraceptives influence endometriosis through two primary mechanisms:
- Hormonal suppression: By reducing estrogen peaks or eliminating ovulation, hormonal methods starve ectopic tissue of the signals it needs to proliferate.
- Endometrial thinning: Continuous hormone exposure thins the uterine lining, reducing the volume of retrograde flow.
Not all contraceptives provide these effects. Understanding each class helps you pick the right tool.

Hormonal Contraceptives That Benefit Endometriosis
Combined oral contraceptive (COC) is a pill that contains both estrogen and progestin, taken in a 21/7 or extended‑cycle regimen. By maintaining steady hormone levels, COCs suppress ovulation and limit estrogen‑driven lesion growth. Clinical studies show a 30‑50% reduction in pain scores after three months of continuous use.
Progestin‑only pill (POP) delivers a low dose of progestin without estrogen. It still inhibits ovulation in most users and directly opposes estrogen's effect on ectopic tissue. POPs are a good alternative for women who experience estrogen‑related side effects such as migraines or breast tenderness.
Levonorgestrel intrauterine device (LNG‑IUD) releases a locally acting progestin. It thins the endometrium, reduces menstrual flow, and has been shown to lessen endometriosis‑related pain in up to 70% of users after six months.
These hormonal methods share the advantage of offering reliable birth control while simultaneously addressing the disease process. However, they may cause side effects such as mood changes, weight gain, or breakthrough bleeding, which need monitoring.
Non‑Hormonal Contraceptives: What They Can and Can’t Do
Copper intrauterine device (Copper IUD) works by creating a hostile environment for sperm. It does not alter hormone levels, so it provides no direct benefit for endometriosis lesions. Some women report unchanged pain levels, while others appreciate the hormone‑free approach, especially if they have contraindications to estrogen or progestin.
Barrier methods-condoms, diaphragms, cervical caps-also lack hormonal impact. They are safe, inexpensive, and protect against sexually transmitted infections, but they do not influence lesion growth.
Special Situations and Considerations
Age and disease stage: Younger women with early‑stage endometriosis often respond well to COCs or POPs. Advanced disease may require a combination of hormonal therapy and surgical excision.
Fertility goals: If pregnancy is desired soon, a progestin‑only method or LNG‑IUD can be stopped without a hormone‑free “wash‑out” period, allowing a quicker return to natural cycles. COCs may need a 1‑2 month break before trying to conceive.
Medical contraindications: Women with a history of clotting disorders, uncontrolled hypertension, or certain migraines should avoid estrogen‑containing pills. In such cases, POPs, LNG‑IUD, or non‑hormonal options become the primary choices.
Side‑effect management: Breakthrough bleeding on hormonal methods is common during the first three months. Using NSAIDs (e.g., ibuprofen) can ease both pain and occasional spotting, but long‑term NSAID use should be discussed with a doctor due to gastrointestinal risk.
Practical Guide: Choosing the Right Contraceptive for Endometriosis
- Assess symptom severity: mild pain may be managed with COCs; severe pain often benefits from an LNG‑IUD or combined surgical‑medical approach.
- Check medical history: estrogen‑related risks push the choice toward progestin‑only or hormone‑free methods.
- Define fertility timeline: if you plan pregnancy within a year, POPs or short‑acting COCs are easier to discontinue.
- Discuss side‑effects: ask your clinician about mood changes, weight impact, or bleeding patterns for each option.
- Schedule follow‑up: re‑evaluate pain scores and lesion size via ultrasound after 3‑6 months of therapy.
Remember, the best method is the one you can stick with consistently while keeping pain under control.
Comparison of Common Contraceptives and Their Impact on Endometriosis
| Method | Hormone Content | Effect on Endometriosis Lesions | Typical Side‑Effects | Duration of Use |
|---|---|---|---|---|
| Combined oral contraceptive (COC) | Estrogen + Progestin | Reduces lesion growth (30‑50% pain reduction) | Breakthrough bleeding, breast tenderness, mood changes | Daily; up to several years |
| Progestin‑only pill (POP) | Progestin only | Suppresses lesions; moderate pain relief | Irregular bleeding, acne, weight fluctuation | Daily; up to several years |
| Levonorgestrel IUD (LNG‑IUD) | Progestin (local release) | Significant pain reduction; slows lesion activity | Spotting first 3‑6 months, cramping | 3-5 years per device |
| Copper IUD | None (non‑hormonal) | No direct effect; symptoms may stay same | Heavy periods, increased cramps | Up to 10 years |
Myth‑Busting: Common Misconceptions
- Myth: Birth control can cure endometriosis.
Reality: Contraceptives manage symptoms and slow progression but do not eradicate existing lesions. Surgery remains the only way to remove them. - Myth: Hormonal pills worsen fertility.
Reality: When stopped, fertility typically returns within a few months. Long‑term use does not diminish ovarian reserve. - Myth: Non‑hormonal methods are safer for everyone.
Reality: While hormone‑free, they provide no relief for endometriosis‑related pain and may be less effective at preventing unintended pregnancy if not used perfectly.
Next Steps and Troubleshooting
If you’ve started a new contraceptive and pain persists after three months, consider these actions:
- Ask your doctor about switching to a higher‑dose progestin IUD.
- Combine hormonal therapy with a short course of GnRH agonists (e.g., leuprolide) for severe cases.
- Track symptoms in a diary; note cycle days, medication timing, and pain intensity to help your clinician fine‑tune treatment.
- Explore adjunct therapies such as pelvic physiotherapy, dietary changes (low‑inflammatory diet), and acupuncture, which many patients report as helpful.
Every woman’s journey is unique. Regular dialogue with a specialist ensures you’re not just managing pain but also preserving reproductive health.
Frequently Asked Questions
Can hormonal birth control prevent endometriosis from developing?
Evidence suggests that long‑term use of combined oral contraceptives or progestin‑only methods can lower the risk of developing new lesions, especially when started shortly after menarche. However, they do not guarantee prevention, and genetics still play a major role.
Is the copper IUD a good choice if I have severe endometriosis pain?
A copper IUD does not address hormone‑driven growth of endometriotic tissue, so most clinicians recommend a hormonal IUD (levonorgestrel) or oral progestins for pain control. The copper device is best reserved for women who cannot take hormones.
How long should I stay on hormonal contraception before I see pain improvement?
Most patients notice a measurable reduction in pelvic pain within 8‑12 weeks of consistent use. If there’s no change after three months, discuss alternative regimens with your doctor.
Will stopping hormonal birth control cause my endometriosis symptoms to flare up?
Discontinuing hormones often leads to a rebound of estrogen levels, which can temporarily increase pain. A gradual taper or switching to a different hormonal method can mitigate this effect.
Are there any natural contraceptive methods that also help with endometriosis?
Natural family‑planning (e.g., fertility awareness) does not modify hormone levels, so it offers no therapeutic benefit for endometriosis. Combining a reliable barrier method with hormone therapy is the most effective strategy.
Understanding the link between contraception and endometriosis puts you in control of both pain and reproductive choices. With the right information and a collaborative doctor, you can find a birth‑control method that eases symptoms while protecting your future plans.

Shawn Simms
October 10, 2025 AT 20:45While the article accurately outlines hormonal mechanisms, it could benefit from clearer citation of the studies supporting the 30‑50% pain reduction claim.
Geneva Angeles
October 13, 2025 AT 10:42I love how the guide breaks down each contraceptive option, but let’s be real – the reality for many of us is far messier than a tidy table can capture.
First, the hormonal suppression you read about isn’t a magic bullet; my friend tried a COC for months and still woke up with excruciating cramps that no pill seemed to dull.
Second, the side‑effects column downplays the emotional roller‑coaster that estrogen can trigger, from mood swings to aggressive irritability that can wreck relationships.
Third, while the LNG‑IUD promises up to five years of relief, the initial spotting can be relentless, turning a simple morning routine into a frantic search for pads.
Fourth, the article mentions “breakthrough bleeding” as a minor nuisance, yet for many patients it becomes a persistent, blood‑soaked nightmare that undermines confidence.
Fifth, the emphasis on “regular follow‑up” ignores the fact that many of us cannot afford frequent specialist visits, leaving us to navigate side effects solo.
Sixth, the claim that “fertility returns quickly” after stopping hormones is overly optimistic; my cousin waited six months of irregular cycles before even getting a positive pregnancy test.
Seventh, there’s a glaring omission of lifestyle adjuncts like diet, physiotherapy, and stress management that can synergize with hormonal therapy.
Eighth, we need to discuss the psychological toll of constantly toggling between birth‑control methods, especially when insurance coverage forces us to jump from a POP to an IUD.
Ninth, the table’s “non‑hormonal methods do nothing” line feels dismissive, because for women with contraindications, a copper IUD might be the only viable birth‑control, even if it doesn’t ease pain.
Tenth, let’s not forget that the “combined oral contraceptive” can exacerbate migraine with aura, a red flag that the guide barely scratches.
Eleventh, the article could benefit from a deeper dive into newer options like the vaginal ring or hormonal patches, which some patients find more tolerable.
Twelfth, the tone sometimes sounds like “pick a pill and you’re done,” neglecting the reality that many cycle through multiple options before finding one that sticks.
Thirteenth, I appreciate the myth‑busting section, but it could be expanded to debunk the belief that “hormonal pills ruin your future fertility” – a myth that still haunts so many.
Finally, your audience deserves a clear, step‑by‑step decision tree that factors in personal budget, side‑effect tolerance, and long‑term reproductive goals, because without that roadmap the guide feels like an impressive brochure rather than a practical lifeline.
Scott Shubitz
October 16, 2025 AT 00:38The hormonal hype is just a circus, and the side‑effects are a horror show that nobody wants to admit.
Lauren Taylor
October 18, 2025 AT 14:35Addressing the theatrical framing of hormonal interventions, it is essential to contextualize the underlying pathophysiology with precise terminological fidelity; endometriotic implants respond to estrogenic signaling cascades, and thus any therapeutic modality that attenuates this axis warrants rigorous mechanistic exposition.
Moreover, clinicians must integrate evidence‑based algorithms that stratify patients by phenotypic severity, comorbid clotting risk, and fertility aspirations, thereby operationalizing a personalized medicine paradigm rather than a one‑size‑fits‑all prescription.
Vanessa Guimarães
October 21, 2025 AT 04:32Oh, thank heavens for yet another glossy brochure that pretends to care while silently ignoring the messy reality of patient experiences.
Lee Llewellyn
October 23, 2025 AT 18:28If you think the guide is the ultimate truth, you’ve clearly never dealt with a stubborn lesion that laughs at our best‑case scenarios.
Drew Chislett
October 26, 2025 AT 07:25I appreciate the thorough breakdown; I’m curious about how quickly fertility returns after stopping an LNG‑IUD.
Rosalee Lance
October 28, 2025 AT 21:22From a philosophical standpoint, the balance between symptom control and reproductive autonomy raises profound questions about bodily sovereignty and the ethical distribution of medical knowledge.
Kara Lippa
October 31, 2025 AT 11:18Great overview; I especially liked the clear table summarising side‑effects.
Puneet Kumar
November 3, 2025 AT 01:15The interdisciplinary approach highlighted here underscores the necessity of integrating gynecologic endocrinology with patient‑centered counseling, ensuring that cultural competency informs contraceptive selection across diverse populations.
michael maynard
November 5, 2025 AT 15:12Sure, pharma loves to push pills, but nobody talks about the hidden agenda behind these ‘miracle’ contraceptives.
william smith
November 8, 2025 AT 05:08Use a progestin‑only method if you have a clotting risk; it avoids estrogen‑related complications.
Timothy Javins
November 10, 2025 AT 19:05I’d argue the evidence for combined oral contraceptives is weaker than the article suggests.
Kay Yang
November 13, 2025 AT 09:02Interesting read 😊
Kristen Moss
November 15, 2025 AT 22:58This American guide ignores the real solutions that work back home.
Rachael Tanner
November 18, 2025 AT 12:55Contrary to popular belief, copper IUDs can aggravate endometriosis in some cases.
Debra Laurence-Perras
November 21, 2025 AT 02:52Consider discussing both hormonal and non‑hormonal options with your doctor.
dAISY foto
November 23, 2025 AT 16:48Yo! thIs guide sH0ws sum cool stuff but u gotta try it out!
Ian Howard
November 26, 2025 AT 06:45Remember, the best contraceptive is the one you’ll actually stick with, no matter how flashy it looks!