When a patient walks in with shortness of breath, fatigue, or swollen ankles, the question isn’t just what’s wrong-it’s how fast can we rule out heart failure? That’s where NT-proBNP blood testing comes in. It’s not just another lab order. For clinicians, it’s the fastest, most reliable way to tell if someone’s heart is struggling-or if something else is causing their symptoms.
Why NT-proBNP Matters More Than You Think
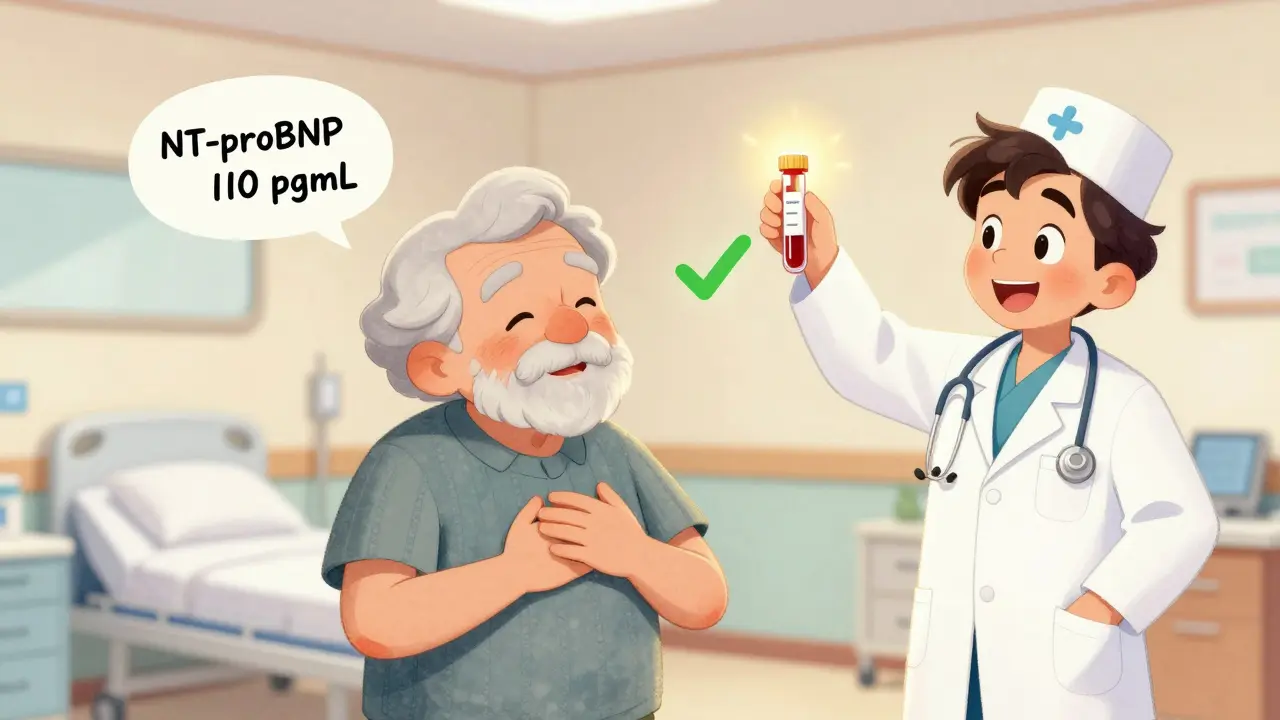
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein released by the heart when its ventricles are stretched from too much pressure or fluid. Think of it like a distress signal. When the heart is under stress-say, from high blood pressure, a past heart attack, or fluid overload-it pumps out more of this marker. The blood test measures how much is floating around. Unlike older tests, NT-proBNP is stable. It doesn’t break down quickly in the tube like BNP does. That means even if there’s a delay in getting the sample to the lab, the result is still accurate. This stability made it the go-to test in hospitals and emergency rooms by the mid-2010s. Today, 68% of all natriuretic peptide tests ordered in the U.S. are NT-proBNP, mostly using Roche’s Elecsys assay. The real power? Its ability to rule out heart failure. If the NT-proBNP level is below 300 pg/mL, the chance that the patient has acute heart failure is less than 2%. That’s not a guess. That’s backed by data from the European Society of Cardiology and confirmed in over 20 clinical studies. For busy ERs and urgent care clinics, that means avoiding unnecessary hospital admissions, echocardiograms, and CT scans-saving time, money, and stress for patients.When to Order NT-proBNP: The 5 Clear Scenarios
You don’t order this test for everyone. It’s not a screening tool. But when used right, it changes outcomes. Here are the five situations where it’s a must:- Patients with new-onset dyspnea-especially those over 50. If someone says they’re out of breath just walking to the bathroom, and you’re not sure if it’s heart failure, COPD, or anxiety-order NT-proBNP. A level under 300 pg/mL makes heart failure extremely unlikely.
- Patients in the emergency department with suspected acute heart failure. The NICE guidelines in the UK and the ESC guidelines in Europe both say: test everyone. A 2022 UK audit showed this reduced unnecessary echocardiograms by 19%.
- Patients with known heart failure who are getting worse. Rising NT-proBNP levels signal worsening disease-even before symptoms get worse. It’s a guide for adjusting diuretics or adding new meds like SGLT2 inhibitors.
- Patients with atrial fibrillation and unexplained symptoms. AFib can mimic heart failure. But if NT-proBNP is normal, you can focus on other causes like thyroid issues or pulmonary embolism.
- Post-ACS (acute coronary syndrome) risk stratification. New 2024 guidelines recommend NT-proBNP testing after a heart attack to predict who’s at highest risk for future events. High levels mean you need tighter follow-up and aggressive therapy.
How to Interpret the Numbers-It’s Not Just One Cutoff
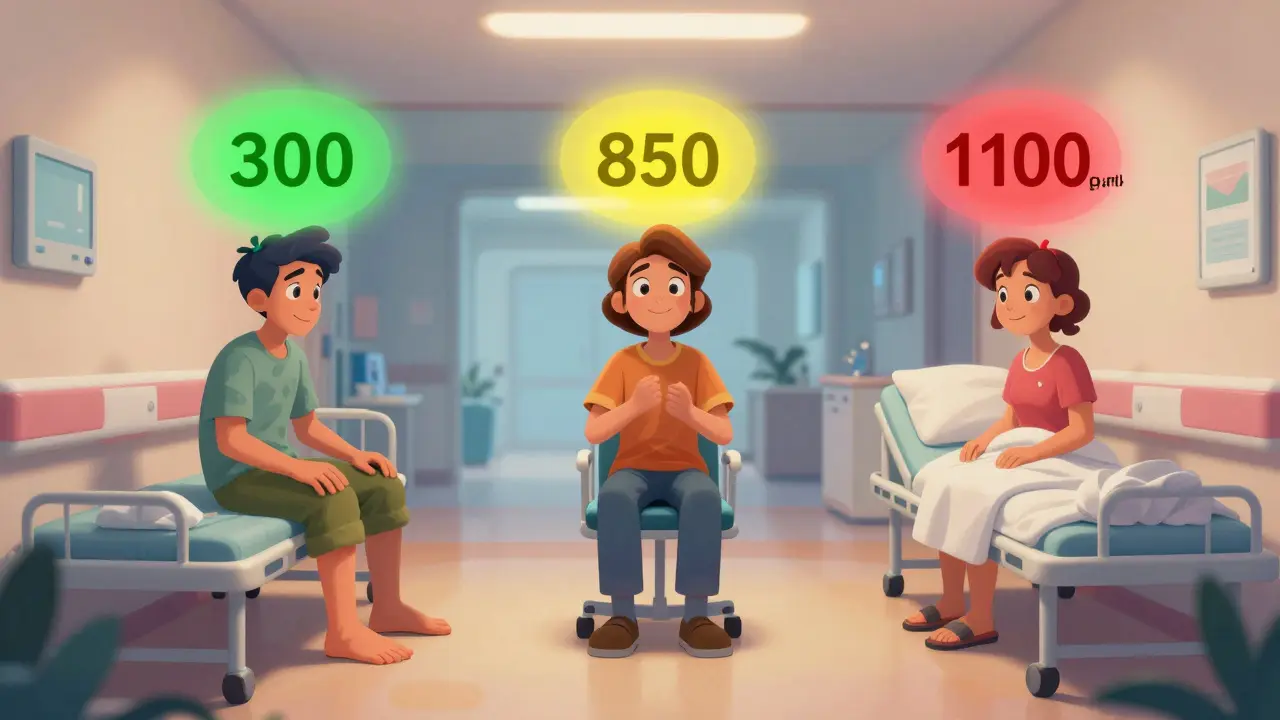
This is where things get tricky. NT-proBNP isn’t a simple yes/no. Age, kidney function, and body weight all change what’s normal.- Age matters. For people under 50, a level above 450 pg/mL raises suspicion. For those over 75, the cutoff jumps to 900 pg/mL. Why? Because NT-proBNP naturally rises about 15-20% every decade-even in healthy people.
- Chronic kidney disease. If someone has stage 3 or worse CKD, their NT-proBNP levels can be 28-40% higher than normal, even without heart failure. Use a higher rule-out threshold: < 1,200 pg/mL for advanced CKD.
- Obesity. Fat tissue suppresses NT-proBNP release. For every 5-point increase in BMI, levels drop 25-30%. So if a heavy patient has a level of 400 pg/mL, that’s actually high for them. Don’t dismiss it.
What NT-proBNP Can’t Do
It’s powerful-but not magic. Here’s where it falls short:- It doesn’t tell you the cause. High levels mean the heart is stressed, but not why. Is it from hypertension? Valvular disease? Myocarditis? You still need imaging and history.
- It’s not for screening healthy people. Medicare data shows 18% of tests are ordered in asymptomatic patients. That’s overuse. No one without symptoms needs this test.
- It can’t replace clinical judgment. A 2021 study in Clinical Chemistry warned that relying solely on NT-proBNP in elderly patients leads to misdiagnosis. One patient had a level of 1,100 pg/mL and was assumed to have heart failure-turns out it was sepsis. The test didn’t lie. The interpretation did.
How the Test Works-And Why It’s Fast
The test needs just 1 mL of blood in a regular serum tube. No fasting. No special prep. Samples stay stable for 72 hours in the fridge and up to six months if frozen. Most hospital labs return results in under an hour. The new point-of-care Roche Cobas h232 device gives results in 12 minutes-ideal for urgent care and rural clinics. The test measures picograms per milliliter (pg/mL). Normal range? That’s the problem. There’s no single “normal.” It’s context-dependent. But analytically, the test is precise: coefficients of variation under 3.5%, sensitivity down to 5 pg/mL, and 99% specificity at established cutoffs.

Phil Hillson
January 18, 2026 AT 19:17Josh Kenna
January 19, 2026 AT 16:57Lewis Yeaple
January 20, 2026 AT 13:59Valerie DeLoach
January 22, 2026 AT 06:44Christi Steinbeck
January 22, 2026 AT 15:08sujit paul
January 23, 2026 AT 10:29Jackson Doughart
January 24, 2026 AT 04:00Jacob Hill
January 24, 2026 AT 19:06