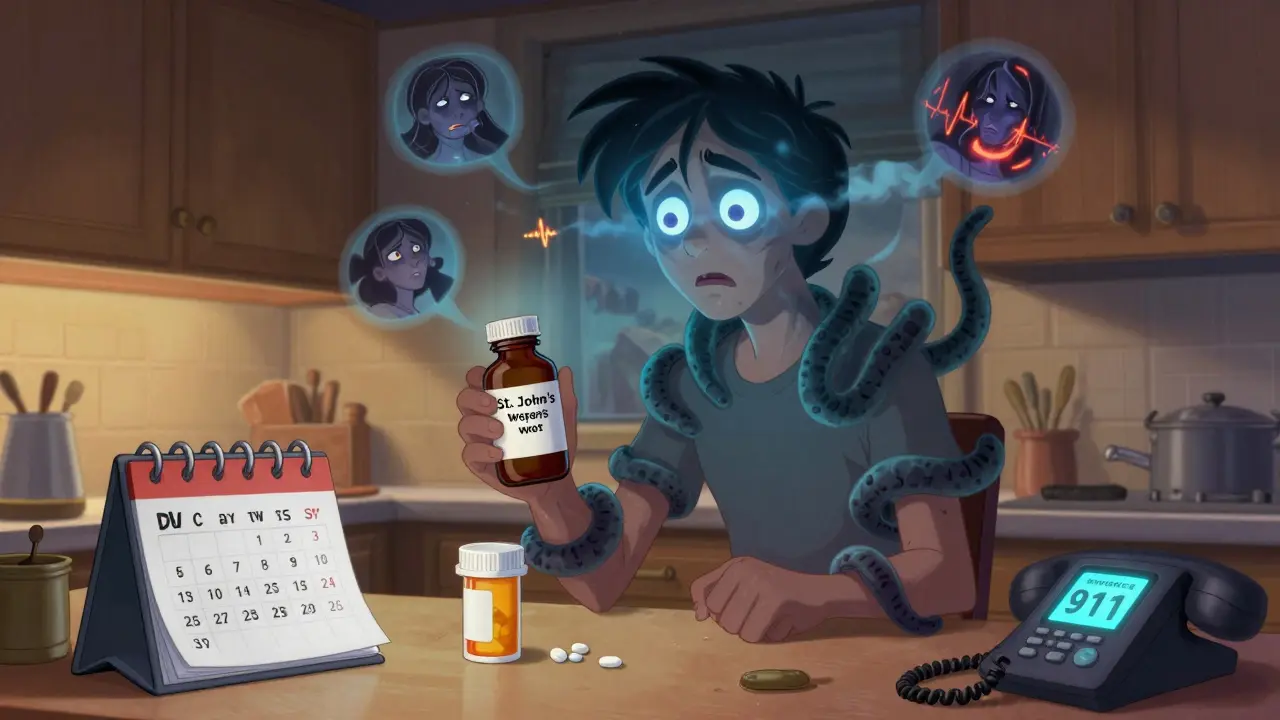
When you start taking an antidepressant, the goal is to feel better-not to end up in the emergency room. But if you take too much, or mix it with another medication, something dangerous can happen: serotonin syndrome. It’s not rare. It’s not theoretical. It’s happening right now to people who thought they were just following their doctor’s instructions.
Imagine this: You’ve been on sertraline for three weeks. Your mood is lifting. Then your back starts to ache, so you pick up a bottle of cough syrup with dextromethorphan. Two hours later, you’re shaking, sweating like you’ve run a marathon, and your heart feels like it’s trying to beat out of your chest. You think it’s the flu. Or anxiety. But it’s not. It’s serotonin syndrome-and it can kill you if you wait too long.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t just an overdose. It’s a toxic buildup of serotonin in your nervous system. Serotonin is a chemical your brain uses to regulate mood, sleep, digestion, and muscle control. Antidepressants like SSRIs and SNRIs work by keeping more serotonin active in your brain. That’s good-until too much piles up.
This isn’t just about taking too many pills. It’s often about mixing medications. Common culprits include:
- SSRIs (like fluoxetine, sertraline, escitalopram)
- SNRIs (like venlafaxine, duloxetine)
- MAOIs (like phenelzine, tranylcypromine)
- Pain meds like tramadol or fentanyl
- Migraine drugs like sumatriptan
- Over-the-counter cough syrups with dextromethorphan
- Some herbal supplements like St. John’s wort
You don’t need to take a massive overdose. Sometimes, just adding one extra drug to your routine is enough. The body doesn’t handle extra serotonin well-and it reacts fast.
The Three Clusters of Warning Signs
Doctors look for three clear patterns when diagnosing serotonin syndrome. If you see even one of these clusters, don’t wait. Call an ambulance.
1. Mental Status Changes
This is where people get confused. They think they’re just anxious or having a panic attack. But it’s more than that.
- Confusion or disorientation (happens in 78% of cases)
- Agitation, restlessness, or extreme irritability (65%)
- Hallucinations or delirium (in severe cases)
- Difficulty concentrating or feeling detached from reality
One patient on Reddit described it like this: “I felt like my brain was short-circuiting. I knew I was scared, but I couldn’t stop shaking or explain why.” That’s not anxiety. That’s your nervous system going haywire.
2. Autonomic Hyperactivity
This is your body’s fight-or-flight system stuck on full blast.
- High blood pressure (systolic over 160 mmHg)
- Fast heart rate (over 100 bpm in 83% of cases)
- High fever (above 38°C / 100.4°F in 67% of cases)
- Profuse sweating (diaphoresis)
- Rapid breathing (over 20 breaths per minute)
- Dilated pupils (5-8mm, compared to normal 2-4mm)
- Nausea, vomiting, or diarrhea (vomiting in 68%, diarrhea in 63%)
These aren’t side effects. They’re signs your body is overheating and under extreme stress. If your temperature climbs above 38.5°C (101.3°F), you’re in danger of organ damage.
3. Neuromuscular Abnormalities
This is the most telling sign-and the one most people miss.
- Tremors (shaking) - the most common early warning (reported in over 80% of cases)
- Muscle twitching or jerking (myoclonus)
- Clonus - rhythmic, involuntary muscle contractions. Try this: gently press your foot downward. If your foot starts bouncing up and down on its own, that’s clonus. It’s the #1 clinical sign of serotonin syndrome.
- Hyperreflexia - your reflexes are way too strong. A doctor taps your knee and your leg kicks hard, way past normal.
- Muscle rigidity - your limbs feel stiff, like they’re locked in place
Clonus and hyperreflexia together? That’s a red flag. In 92% of confirmed cases, clonus is present. If you see this, don’t text your friend. Don’t Google it. Call emergency services.
How Fast Does It Happen?
It doesn’t creep up. It hits hard and fast.
- 30% of people show symptoms within 1 hour
- 60% develop symptoms within 6 hours
- 90% show signs within 24 hours
That’s why so many people get misdiagnosed. They think it’s food poisoning. Or a panic attack. Or the flu. But if you started a new medication or added something to your routine in the last 24 hours, and you’re shaking, sweating, and your reflexes are wild-serotonin syndrome is the most likely cause.

What Happens If You Ignore It?
Serotonin syndrome can go from mild to life-threatening in hours.
Severe cases include:
- Body temperature above 41.1°C (106°F)
- Seizures
- Irregular heartbeat (arrhythmias)
- Unconsciousness
- Multi-organ failure
Death occurs in 0.5% to 12% of cases-mostly from extreme fever or muscle breakdown (rhabdomyolysis), which floods your kidneys with toxic proteins. The faster you get help, the better your chance.
How Doctors Diagnose It
There’s no blood test that confirms serotonin syndrome. No scan. No lab value. Diagnosis is based on symptoms and medication history.
The gold standard is the Hunter Serotonin Toxicity Criteria. You need one of these:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus + agitation or sweating
- Tremor + hyperreflexia
- Muscle rigidity + fever + ocular or inducible clonus
If you meet one of these, you have serotonin syndrome. That’s it. No waiting for labs. No second opinions. Treat it now.
What to Do If You Suspect It
Time is everything.
- Stop taking all serotonergic medications immediately. Don’t wait for a doctor. If you’re on an SSRI and took tramadol, stop both.
- Call emergency services or go to the ER. Don’t drive yourself if you’re confused or having muscle spasms.
- Don’t try to “wait it out.” This isn’t a bad day. It’s a medical emergency.
- Tell the ER team exactly what you took, when, and how much. Include supplements, OTC meds, and even herbal teas.
In the hospital, treatment includes:
- Benzodiazepines (like lorazepam) to calm muscle spasms and agitation
- IV fluids to prevent dehydration from vomiting and sweating
- External cooling (ice packs, cooling blankets) to bring down fever
- Cyproheptadine, an antidote, given orally or through a tube if symptoms are severe
Most people recover within 24 to 72 hours if treated early. But delays can be fatal.
How to Prevent It
The best way to avoid serotonin syndrome? Know what you’re taking.
- Never mix antidepressants with other serotonergic drugs without a doctor’s approval. Even “safe” OTC meds can trigger it.
- If you’re switching from an MAOI to an SSRI, wait at least 14 days. The FDA requires this. Don’t skip it.
- Keep a full list of all medications and supplements. Bring it to every appointment-even if you think it’s “just a cough syrup.”
- Ask your pharmacist or doctor: “Could this interact with my antidepressant?” Don’t assume they know. Most don’t unless you ask.
- Be extra careful when starting a new antidepressant. The first 2-4 weeks are the highest risk period.
Studies show that when patients are educated about interactions, the risk drops by nearly half. Knowledge saves lives.
Why This Is More Common Than You Think
Between 2015 and 2022, reported cases of serotonin syndrome in Australia and New Zealand rose by 38%. Why? More people are on antidepressants. More people are taking multiple meds for chronic pain, migraines, or anxiety. And many doctors don’t ask about OTC drugs or supplements.
Over 78% of cases involve two or more serotonergic drugs. SSRIs cause 62% of cases. SNRIs, 24%. MAOIs, 8%. But it’s not just about the drug-it’s about the combination.
And here’s the scary part: 25% of cases are missed by doctors. They think it’s anxiety, the flu, or a psychiatric episode. That’s why you need to know the signs.
Final Warning: Don’t Wait for a Second Symptom
Shaking? Sweating? Fast heartbeat? That’s not stress. That’s your body screaming for help.
Serotonin syndrome doesn’t care if you’re “just taking a little extra.” It doesn’t care if you thought the cough syrup was harmless. It doesn’t care if you’ve been on your antidepressant for months. If you added something new-and now you feel off-act now.
It’s not paranoia. It’s science. And it’s happening to people just like you.
Can serotonin syndrome happen with just one antidepressant?
Yes, but it’s rare. Most cases happen when two or more serotonergic drugs are combined. However, taking a very high dose of a single SSRI or SNRI-especially in someone who’s sensitive or has liver problems-can still trigger serotonin syndrome. It’s less common than drug interactions, but it’s possible.
Is serotonin syndrome the same as neuroleptic malignant syndrome (NMS)?
No. They’re often confused, but they’re very different. NMS usually develops over days or weeks, often after starting antipsychotic meds. It causes slow, stiff muscles (rigidity), low fever, and slowed reflexes. Serotonin syndrome happens fast-within hours-and causes jerky muscles, high fever, and overactive reflexes. Clonus and hyperreflexia are hallmarks of serotonin syndrome and don’t occur in NMS.
Can I check my serotonin levels to know if I have serotonin syndrome?
No. There’s no reliable blood test for serotonin syndrome. Serotonin levels in the blood don’t match what’s happening in your brain and nervous system. Diagnosis is based entirely on symptoms and medication history using the Hunter Criteria. Don’t rely on lab tests-watch your body.
What should I do if I accidentally took two serotonergic drugs?
Stop both medications immediately. Monitor yourself closely for the next 6-24 hours. Watch for tremors, sweating, rapid heartbeat, or confusion. If any symptoms appear, go to the ER. Don’t wait. Even if you feel fine now, symptoms can start suddenly. It’s better to be safe than sorry.
Are some antidepressants riskier than others?
SSRIs like sertraline and fluoxetine are involved in the most cases because they’re so widely prescribed. SNRIs like venlafaxine carry higher risk when combined with other drugs because they affect both serotonin and norepinephrine. MAOIs are the most dangerous to mix-they require strict waiting periods. But any serotonergic drug can contribute to serotonin syndrome when combined with another.
Can I use ibuprofen or acetaminophen if I’m on an antidepressant?
Yes. Regular painkillers like ibuprofen and acetaminophen don’t increase serotonin and are generally safe. But avoid tramadol, codeine, or certain cold medicines with dextromethorphan. Always check labels or ask a pharmacist before taking anything new.
How long does it take to recover from serotonin syndrome?
If caught early, most people recover within 24 to 72 hours after stopping the medication and getting treatment. Severe cases may take longer, especially if there’s organ damage. Recovery is almost guaranteed with prompt care. Delayed treatment increases the risk of complications or death.
Should I avoid antidepressants altogether because of this risk?
No. Antidepressants save lives. The risk of serotonin syndrome is low if you take them as prescribed and avoid dangerous combinations. The real danger is not knowing the signs. If you’re on an antidepressant, learn the symptoms, talk to your doctor about all your medications, and never ignore sudden changes in how you feel.


Prakash Sharma
January 9, 2026 AT 06:55Bro, I saw this happen to my cousin in Delhi. He took Zoloft and some cough syrup for his cold. Thought he was just having a panic attack. Ended up in ICU for three days. No one warned him. Doctors in India don't even ask about OTC meds. This post saved my life. Share this with everyone.
Donny Airlangga
January 9, 2026 AT 15:11I’m a nurse in Chicago and I’ve seen this too many times. People think ‘it’s just a little extra’-but serotonin syndrome doesn’t care. One guy mixed fluoxetine with tramadol for back pain. Walked in sweating, shaking, pupils like saucers. We had to intubate him. Please, if you’re on antidepressants, keep a list of everything you take. Even that ‘natural’ supplement.
swati Thounaojam
January 10, 2026 AT 22:45just took sertraline last week. now im paranoid about every cold med. thanks for the scare.
Aubrey Mallory
January 11, 2026 AT 07:10Look, I get it. People don’t read labels. But this isn’t just about meds-it’s about how we treat mental health like it’s a quick fix. You don’t pop pills and forget. You learn. You ask. You pay attention. If you’re too lazy to read the fine print, don’t blame the system when your body rebels. This is basic responsibility. And if you’re on an SSRI and still taking St. John’s wort? You’re not brave. You’re reckless.
Dave Old-Wolf
January 11, 2026 AT 19:00So if I take ibuprofen with my antidepressant, I’m good? What about melatonin? Or that gummy vitamin with B6? I’m trying to be careful but I don’t know what’s safe anymore. Can someone make a simple list? Like, green light, yellow light, red light stuff?
Ken Porter
January 11, 2026 AT 20:26Wow. Another fear-mongering post from the mental health industrial complex. People are dying from antidepressants? Newsflash: they’re not magic. They’re chemicals. And if you can’t handle that, maybe don’t take them. Also, dextromethorphan? It’s in cough syrup. People have been taking it since the 80s. Maybe the problem isn’t the meds-it’s the paranoia.
Manish Kumar
January 13, 2026 AT 07:56Think about it: serotonin isn’t just a neurotransmitter-it’s the soul’s chemical signature. When we flood it, we’re not just overloading a system, we’re violating the natural rhythm of being. Modern medicine treats the body like a machine, but the mind? The mind is a temple. And when we pour synthetic chemicals into it without reverence, we invite chaos. This isn’t just medical-it’s metaphysical. The body screams because the spirit knows something’s wrong. We’ve forgotten how to listen. We’ve outsourced our intuition to pharmacists and algorithms. And now we’re paying the price-in tremors, in fever, in the quiet horror of not knowing if it’s anxiety… or the end.
Molly Silvernale
January 14, 2026 AT 05:18It’s like your nervous system is a Wi-Fi router that got hit by a lightning storm-suddenly everything’s flashing, crackling, disconnecting… and you’re just sitting there thinking, ‘Huh, my phone’s acting weird.’ But no-it’s the whole house on fire. And the fire alarm? It’s your shaking hands. Your racing heart. Your wild eyes. You don’t need a test. You need to trust your body. And if you don’t? Then you’re already too late.
Kristina Felixita
January 14, 2026 AT 06:13so i was on lexapro and took some cold meds last winter… i thought i was just really anxious but my hands were like… vibrating? like a phone on silent? and i was sweating so much my shirt stuck to my back. i went to urgent care and they said ‘it’s just stress.’ i cried in the parking lot. i wish i’d known then what i know now. thank you for this. please share this with your grandma. she’s probably taking st. john’s wort and a pill for her depression and doesn’t even know the names.
Joanna Brancewicz
January 14, 2026 AT 06:49Clonus is the key diagnostic marker. Hyperreflexia + tremor = high probability. Hunter Criteria sensitivity is 97%. Don’t rely on labs. Rely on clinical signs. If clonus is present, initiate treatment immediately. Benzodiazepines first-line. Cyproheptadine if severe. Time is brain. Time is muscle. Time is life.
Evan Smith
January 15, 2026 AT 16:16So let me get this straight… I can’t take NyQuil with my Zoloft? But I can take it with my coffee? What’s next, can I mix my antidepressant with a Red Bull? I’m just trying to survive Monday. Is there a chart? Like, ‘Things That Won’t Kill You (Probably)’?
Lois Li
January 17, 2026 AT 04:35I’m so glad someone wrote this. I used to think my tremors were just nerves. Turns out I was mixing venlafaxine with a migraine med. My doctor didn’t even ask about the sumatriptan. I almost didn’t make it. Now I keep a printed list of everything I take in my wallet. I give copies to my friends. Knowledge isn’t power-it’s survival. And we owe it to each other to share it.
christy lianto
January 17, 2026 AT 20:20My sister had serotonin syndrome after taking Wellbutrin and a new pain cream. She was fine one day, in the ER the next. They said she was lucky. I’m telling everyone I know: if you feel off after adding anything new-anything-GO TO THE HOSPITAL. Don’t wait. Don’t Google. Don’t text your friend. Call 911. Your life isn’t worth the risk.
Luke Crump
January 18, 2026 AT 16:02This whole post is a scam. Serotonin syndrome? Sounds like a marketing ploy by pharma to scare people into buying more drugs. If you’re shaking and sweating, maybe you’re just having a panic attack because you’re scared of your own medication. Maybe the real problem isn’t serotonin-it’s the fear of taking antidepressants at all. Wake up. You’re being manipulated.